Medical Coding Compliance: Reducing Errors and Denials
Are rising claim denials slowing down reimbursements and adding pressure on billing operations? When coding or documentation gaps interrupt payments, teams spend hours reworking claims that should have been paid the first time. This is where medical coding compliance becomes essential, not only for accuracy but for financial reliability.
The trend is concerning. In 2024, the initial denial rate increased by 2.4%, reaching 11.81%, highlighting how preventable errors continue to impact revenue across healthcare settings. This puts added responsibility on compliance, audit, and revenue cycle functions to strengthen oversight and reduce avoidable denials.
This blog covers what medical coding compliance is, why audits matter, how they help reduce denials, and how newer tools are improving accuracy and oversight.
Key Takeaways
- Coding compliance supports revenue integrity by reducing preventable denials tied to documentation and rule errors.
- Audits reveal where coding accuracy breaks down and help organizations apply corrective action before claims reach payers.
- Strong audit programs rely on targeted sampling, transparent reporting, and alignment with current payer and regulatory standards.
- Most challenges arise from shifting guidelines, specialty complexity, and inconsistent clinical documentation.
- Automation, data visibility, and rule maintenance now play a central role in sustaining compliance over time.
Table of Contents
- What is Medical Coding Compliance?
- Why Healthcare Coding and Compliance Audits Matter
- How Coding Compliance Audits Reduce Denials
- How Medical Coding Audits Are Conducted
- Challenges and Best Practices for Coding Compliance
- How RapidClaims Automates Compliance to Reduce Errors and Denials?
- Wrapping Up
- FAQs
What is Medical Coding Compliance?
Medical coding compliance refers to how accurately clinical encounters are translated into standardized codes while meeting payer policies, regulatory requirements, and documentation expectations.
It ensures that ICD-10, CPT, HCPCS, and HCC assignments reflect what was actually documented, protect reimbursement integrity, and withstand audit scrutiny.
True compliance is not just correct coding; its alignment with changing guidelines, specialty nuances, and revenue cycle accountability.
Because payment accuracy depends on how well compliance is monitored, healthcare organizations turn to coding and compliance audits to assess performance, identify risks, and track improvement.
Why Healthcare Coding and Compliance Audits Matter
Audits give healthcare organizations visibility into how coding decisions affect reimbursement, clinical reporting, and regulatory exposure. They help leaders understand whether coding accuracy supports payment integrity or introduces denial risk.
They matter because audits help organizations:
- Quantify reimbursement leakage caused by inaccurate coding or missing documentation.
- Detect payer-specific compliance gaps before they trigger recoupments or penalties.
- Validate coding alignment across specialties, encounter types, and risk models.
- Identify coder education needs tied to HCC shifts, E&M changes, or LCD/NCD updates.
- Improve Risk Adjustment Factor (RAF) capture accuracy for value-based reimbursement and Medicare Advantage plans.
These audit findings set the stage for understanding how compliance activities directly reduce denials and strengthen financial performance.
How Coding Compliance Audits Reduce Denials
For organizations managing complex reimbursement workflows, denials often signal deeper issues in documentation quality, coding interpretation, or payer rule alignment. Compliance audits help find these gaps before they translate into payment delays or corrective action requests.
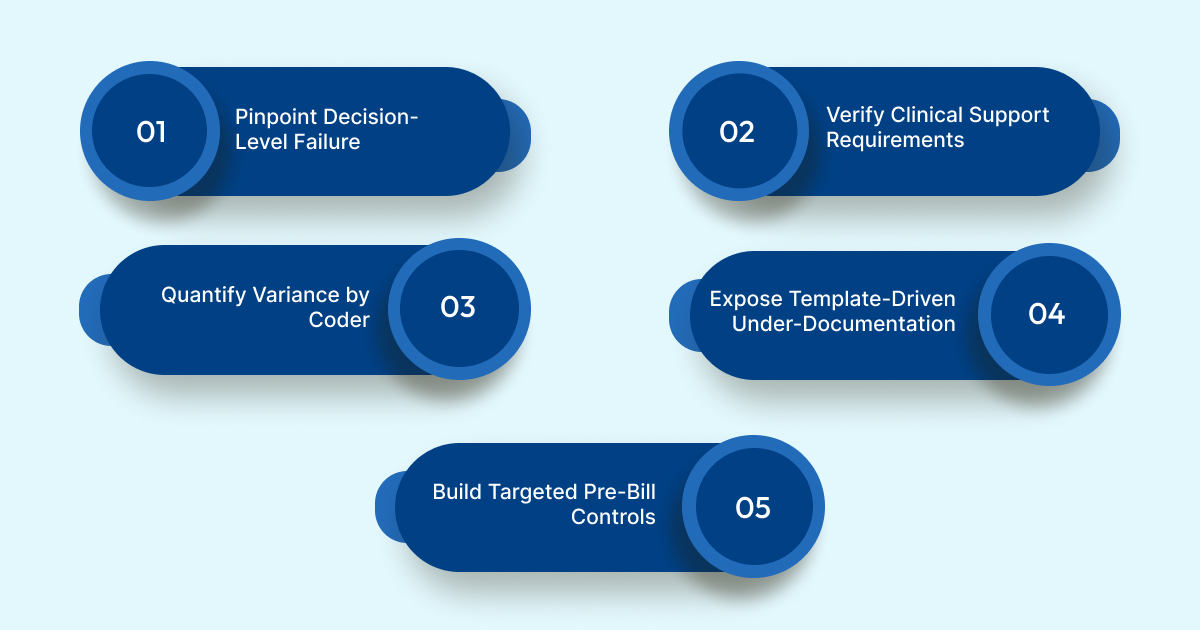
Audits reduce denials by enabling organizations to:
- Pinpoint Decision-Level Failure: Trace denials back to where the coding decision went wrong, whether a missed complication code changed DRG assignment, an incorrect HCC selection suppressed RAF, or a modifier error triggered NCCI edits.
- Verify Clinical Support Requirements: Evaluate whether diagnoses meet payer documentation thresholds (e.g., chronic condition recurrence, specificity qualifiers, or time-based E&M elements), which scrubbers alone typically miss.
- Quantify Variance by Coder or Specialty: Compare audit outcomes across coders, service lines, and encounter types to reveal where interpretation drift creates systematic revenue risk.
- Expose Template-Driven Under-Documentation: Audit review often shows that note templates omit exam, history, or assessment detail required for higher E&M levels, leading to avoidable underpayments or level-down denials.
- Build Targeted Pre-Bill Controls: Convert audit patterns into targeted edits such as HCC validation rules, DRG shift checks, or medical necessity prompts rather than generic claim edits.
Struggling to turn audit findings into measurable denial reduction? RapidClaims embeds rules, documentation logic, and denial risk scoring directly into coding workflows, helping compliance teams prevent repeat errors instead of just reporting them.
Instead of functioning as scorecards, effective audits act as diagnostic systems, which becomes clearer once we look at how medical coding audits are structured and operationalized.
Also Read: How to Effectively Appeal a Denied Insurance Claim: A Step-by-Step Guide
How Medical Coding Audits Are Conducted
Coding audits are structured review cycles that evaluate coding accuracy, documentation sufficiency, and reimbursement integrity. Their value depends not on sampling volume, but on how findings feed operational changes.
1. Start With an Audit Objective
Audits begin with a clear objective, targeting risk adjustment accuracy, DRG shifts, E&M leveling, or a payer-specific denial trend. Scoping determines what the audit will measure and why.
2. Select Audit Samples Based on Risk
Charts are chosen using risk criteria for high-complexity cases, historically denied claims, encounters tied to chronic condition coding, or service lines with variance. This avoids random auditing and directs effort where revenue exposure is highest.
3. Assign Records for Independent Code Review
A different reviewer re-codes each chart from scratch using current ICD-10, CPT, HCPCS, and payer rules. The separation between original coding and audit review is what reveals interpretation differences.
4. Compare Audit Codes With Original Coding Output
Auditors analyze exactly where the outputs differ, missed severity qualifiers, unsupported diagnoses, modifier issues, or inaccurate E&M levels. This comparison identifies decision-level failure, not general error rates.
5. Validate Documentation Against Billing Requirements
Auditors check whether the note contains the clinical elements needed to support code specificity, medical necessity indicators, time-based criteria, or chronic condition recurrence. Unsupported coding is classified as documentation failure.
6. Classify Findings Into Actionable Groups
Instead of counting errors, findings are categorized: documentation gap, rule misapplication, risk capture miss, provider practice variance, or template-driven omission. Categorization enables focused remediation.
7. Send Findings to Those Who Can Fix Them
Issues go to the right recipients, provider education, coding leaders, CDI teams, compliance owners, or IT teams when templates or rule sets need modification. This prevents audit results from remaining theoretical.
8. Implement Corrections Inside Daily Workflow
Organizations update note prompts, refine reference guides, revise payer edit logic, instruct provider groups, or adjust coding checklists. This embeds improvement into work, not just into a report.
9. Re-Audit to Confirm Improvement
Teams repeat focused reviews to verify whether corrections changed coding behavior, denial rates, RAF accuracy, or DRG integrity. This makes the audit cycle continuous rather than episodic.
This step-driven approach works only when teams can maintain accuracy and consistency over time. That's where most organizations encounter obstacles, making it important to understand the challenges and best practices in coding compliance.
Also Read: Robotic Process Automation and AI in Healthcare Operations.
Challenges and Best Practices for Coding Compliance
Maintaining compliance is complex because accuracy depends on shifting rules, documentation behaviors, and reviewer consistency. Organizations succeed when they focus on addressing operational barriers, not just scoring accuracy.
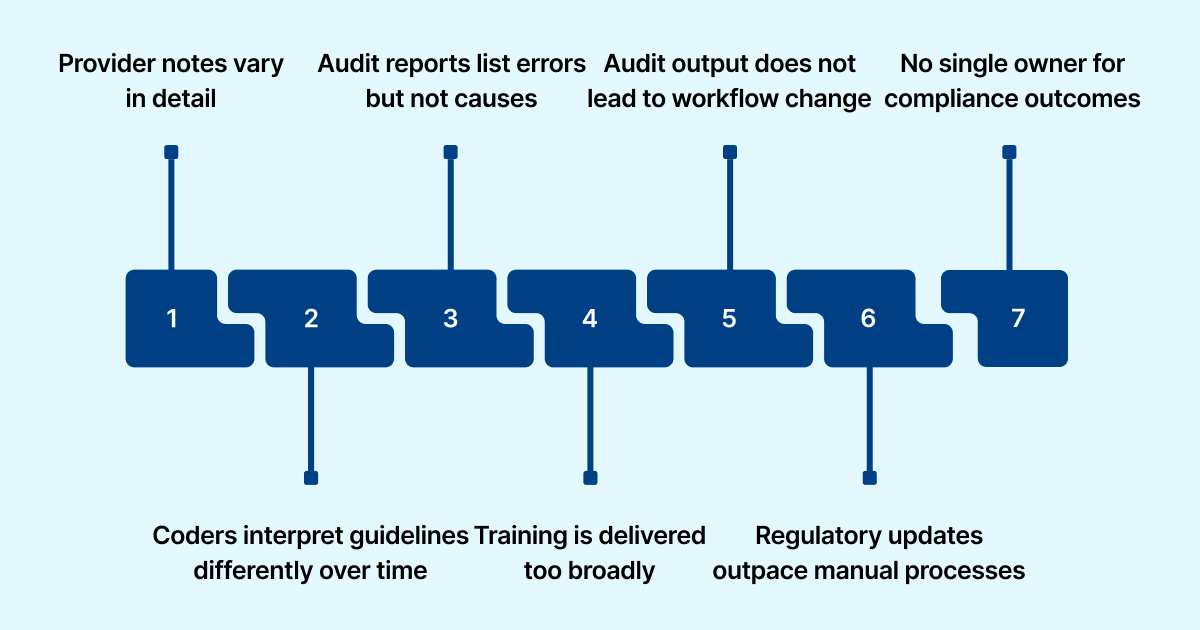
Key Challenges and Practical Best Practices:
- Provider notes vary in detail and structure: Embed mandatory fields or prompts (e.g., disease severity, exam elements, staging) to ensure coders get the specificity required to support codes.
- Coders interpret guidelines differently over time: Run periodic side-by-side case reviews where coders justify assignments to realign interpretation before inconsistency drives denials.
- Audit reports list errors but not causes: Tag findings to root drivers. Documentation gap, rule misapplication, and unsupported diagnosis, so remediation maps to the correct owner and workflow.
- Training is delivered too broadly: Build micro-training tied to audit trends (e.g., modifier misuse in orthopedics, HCC capture gaps in primary care) rather than generic refreshers.
- Audit output does not lead to workflow change: Convert patterns into operational fixes, update templates, revise coding job aids, adjust medical necessity checklists, or add pre-bill checkpoints.
- Regulatory updates outpace manual processes: Establish structured update cycles for CMS, HCC, NCCI, and payer rules or use systems that auto-synchronize rule sets to avoid lag-based errors.
- No single owner for compliance outcomes: Assign ownership for documentation quality, coding accuracy, rule maintenance, and reporting so issues do not sit unresolved between departments.
These gaps show why organizations struggle to sustain compliance through manual processes alone. This is where automation strengthens oversight, reduces error exposure, and improves denial prevention.
How RapidClaims Automates Compliance to Reduce Errors and Denials?
RapidClaims is an AI-driven platform that automates medical coding, improves operational efficiency, and reduces administrative overhead. It strengthens reimbursement outcomes by keeping coding output aligned with current healthcare regulations.
With up to a 70% drop in preventable denials and A/R recovery accelerated by 5 days, the platform delivers measurable financial gains.
- AI-Powered Medical Coding with RapidCode: RapidCode automates medical coding, processing 1000+ charts per minute, reducing coding errors, preventing denials, and accelerating reimbursements. It lifts coder productivity by 170% while maintaining accuracy.
- Real-Time Data Scrubbing with RapidScrub: RapidScrub ensures compliance by scrubbing clinical data before submission, verifying it against payer-specific rules and reducing denial risk. It helps detect issues early, preventing errors and ensuring faster claims processing.
- Risk Adjustment and Clinical Documentation with RapidCDI: RapidCDI transforms clinical documentation into precise risk scores at the point of care, improving coding efficiency, boosting HCC capture by 24%, and saving 30 minutes per day per MD. This leads to an additional $2.2M in annual revenue gains.
With coding automation, AI-guided workflows, and real-time intelligence, RapidClaims supports accuracy and consistency across the claims lifecycle.
Wrapping Up
Compliance-driven coding helps healthcare organizations improve accuracy, reduce preventable denials, and maintain reimbursement confidence. When workflows align with guidelines and documentation expectations, teams spend less time reworking claims and more time improving financial performance.
RapidClaims supports this by automating coding, applying rule logic consistently, and providing transparent, audit-ready outputs that make compliance easier to sustain.
See how RapidClaims strengthens coding compliance and denial prevention. Schedule a Free Demo.
FAQs
1. How often should healthcare organizations perform coding compliance audits?
A. Most organizations conduct quarterly or biannual audits, but high-volume specialties or value-based care programs may require monthly reviews to stay aligned with payer updates.
2. Who is typically responsible for maintaining coding compliance in a provider group?
A. Compliance teams, coding managers, and revenue cycle leaders share ownership, with auditors validating output and IT teams supporting technology alignment.
3. Does coding compliance apply to outsourced billing vendors as well?
A. Yes, provider organizations remain accountable for accuracy even if billing is outsourced, so vendors must follow internal compliance policies and audit expectations.
4. Can automation replace internal auditors?
A. No, automation improves audit workflows by reducing manual effort and spotting risk patterns, while auditors still validate judgment-based scenarios and guide corrective actions.
5. Which specialties face the highest coding compliance risk?
A. High-variance areas like cardiology, oncology, and behavioral health often see high risk due to growing guidelines, multi-code encounters, and complex documentation dependencies.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








