.webp)
Basics of Using 95 Modifier in Telehealth Services Billing


Telehealth has become essential to healthcare, especially after the global pandemic. More and more patients prefer the convenience of care from home, and healthcare providers are stepping up to meet that demand with virtual visits.
But here's the thing: billing can get tricky with this shift to telemedicine. Understanding how to use the correct modifiers and CPT codes is critical to ensure you're appropriately reimbursed for your services.
One of the key modifiers to keep an eye on is the 95 modifier—knowing how and when to use it can help ensure your claims get processed correctly and paid out without issues. In this blog, we'll break down everything you need to know about using the 95 modifier for telehealth billing—from when to use it, to common mistakes, to how it can help you get reimbursed faster. Here’s a quick overview of what we’ll cover:
What is the 95 Modifier and Why It Matters in Telehealth Billing?
The 95 modifier is essential when it comes to billing for telehealth services. This modifier tells insurers that your service is delivered via real-time, interactive audio and video technology, making it eligible for reimbursement, just like an in-person visit.
Why does it matter? Insurance companies need clear, accurate information about how services are delivered.
Since telehealth is still relatively new for many payers, using the 95 modifier ensures that your claim isn't rejected or flagged as an inappropriate service for reimbursement. Without it, you risk losing out on payments for the care you've already provided.
In short, the 95 modifier helps you get paid for telehealth services by confirming that the consultation is happening in real-time, and it's recognized as equivalent to an in-person visit for billing purposes.
This is especially important as more insurers adapt to the changing landscape of healthcare delivery.
When Should You Use the 95 Modifier in Telehealth Claims?
Knowing when to use the 95 modifier is crucial for approving your claims. It's not just about adding the modifier to every telehealth service; it has to meet specific criteria. Here's a breakdown of when it's appropriate to use:
1. Real-Time, Interactive Communication
The 95 modifier should only be used when the telehealth consultation occurs in real-time, meaning there's live interaction between the healthcare provider and the patient.
This could be through video calls, two-way audio, or other interactive technology that allows for immediate exchange of information. If the communication is asynchronous (like email or recorded videos), the 95 modifier doesn't apply.
2. Eligible CPT Codes
The service you're billing for must be eligible for telehealth reimbursement. This includes most established office visits, consultations, or follow-up care.
Ensure you're using the correct CPT codes for telehealth, which vary depending on the service provided.
3. Payer Requirements
Different insurance companies have specific guidelines about when the 95 modifier should be used.
For example, Medicare and Medicaid have clear telehealth rules, but private insurers may have slightly different policies. Always double-check payer guidelines to avoid claim denials.
Suppose a doctor schedules a video consultation to discuss a patient's ongoing treatment plan for chronic hypertension. In that case, the 95 modifier should indicate that the consultation was live and interactive.
However, if the doctor simply emails the patient follow-up instructions or sends a pre-recorded video explaining their medication, the 95 modifier wouldn't apply, as it's not a live interaction.
When in doubt, it's better to add the 95 modifier than leave it out, especially if you're unsure whether the service qualifies as telehealth. But remember, it's only applicable to those live, interactive sessions with your patient.
Common Mistakes in Using the 95 Modifier (and How to Avoid Them)?

Even experienced healthcare providers and billing specialists can make mistakes using the 95 modifier.
A small error can lead to claim denials or delayed payments, so it's essential to be aware of common pitfalls. Here are some mistakes to watch out for and tips on how to avoid them:
1. Confusing the 95 Modifier with Other Modifiers
Mixing up the 95 modifier with others, especially the GT modifier, is easy. While both relate to telehealth, the 95 modifier is explicitly used for real-time, interactive services, whereas the GT modifier was previously used.
Using the wrong one could result in a claim rejection. Be sure you know which modifier is required for each service.
2. Using the 95 Modifier for Non-Telehealth Services
One of the biggest mistakes is applying the 95 modifier to in-person services. This modifier is intended only for telehealth, so if you use it when a patient is physically present, your claim will likely be denied.
Only apply the 95 modifier when the consultation is delivered remotely in real-time.
3. Forgetting to Check the Payer Guidelines
Each payer has different expectations for how telehealth services should be billed. Some may have additional requirements or restrictions on using the 95 modifier, and failing to follow these specific guidelines could cause claim issues.
Always check the payer's rules to ensure your claims are submitted correctly.
Avoiding these common mistakes can help you keep track of claims and reduce the chances of delays or rejections.
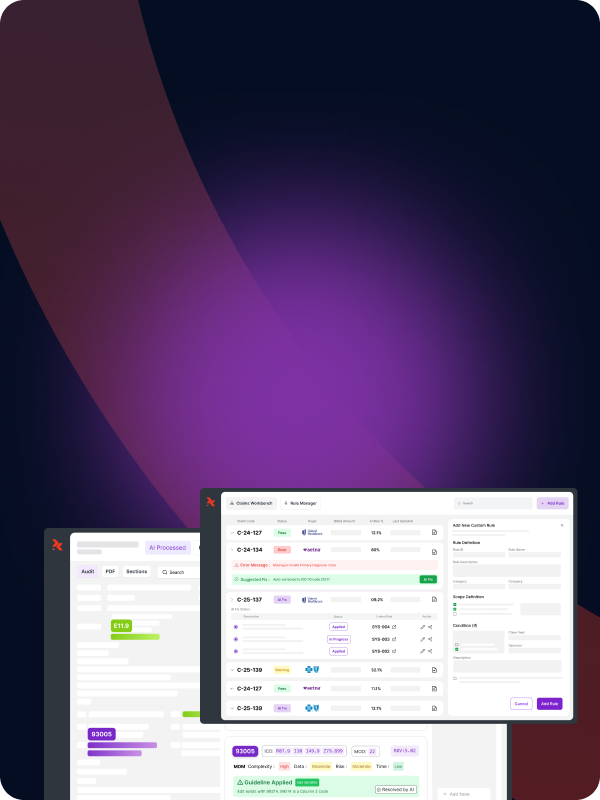
RapidClaims helps reduce telehealth claim errors by flagging missing modifiers and validating CPT code usage during the coding process, helping you avoid common pitfalls.
Key Payer Guidelines for the 95 Modifier You Should Know
Understanding payer-specific guidelines is essential when using the 95 modifier for telehealth services. Each insurer, from government programs like Medicare and Medicaid to private insurance companies, has its own set of rules.
While the 95 modifier is widely recognized, there are nuances in how it should be applied based on the payer's requirements. Ensuring compliance with these guidelines can significantly reduce the risk of claim denials and delays, helping you get reimbursed for your telehealth services efficiently.
Here's a quick overview of what you need to know about the 95 modifier for different types of payers:
How to Make Modifier 95 Work for You: Tips for Better Reimbursement
Now that you know what the 95 modifier is and how to use it correctly, it's time to ensure you're getting the most out of it.
Proper use of the 95 modifier doesn't just ensure that your claims are processed correctly—it can also help boost reimbursement rates and reduce claim denials.
Here are some practical tips to ensure you're using the 95 modifier to its fullest potential:
1. Double-Check Payer Requirements
Every insurer has specific rules for telehealth billing, so before submitting a claim, ensure you're familiar with the requirements for the 95 modifier.
Even small details, like whether a specific form or a particular CPT code is required, can make a big difference in getting your claim approved.
2. Keep Documentation Organized
For telehealth visits, proper documentation is essential. Be sure to keep a clear record of the service, technology, and patient consent (if required).
Insurers may request additional documentation to prove that the consultation was conducted via telehealth, so being organized can speed up the reimbursement process.
3. Use the Right CPT Codes
The 95 modifier must use the correct CPT code for telehealth services. Incorrect CPT codes or missing codes can cause your claims to be delayed or denied.
Make sure you're using the most up-to-date codes and that they align with the service provided. Keeping a list of telehealth-specific CPT codes can save you time and prevent mistakes.
4. Automate and Streamline Billing
Using a platform like RapidClaims.ai can help simplify your telehealth billing process. With automated tools to track and submit claims accurately, you can ensure that modifiers and CPT codes are applied correctly.
This reduces manual errors, speeds up claim submissions, and ultimately helps improve reimbursement rates.
Following these tips can improve your chances of timely and accurate reimbursement for telehealth services. With the right tools and processes, you can avoid common pitfalls and focus on providing excellent care.
RapidClaims supports accurate telehealth coding by offering real-time code and modifier suggestions, helping you submit cleaner claims with fewer errors.
Conclusion
Navigating the world of telehealth billing doesn't have to be a headache. By understanding when and how to use the 95 modifier, you can ensure that your claims are processed smoothly and appropriately.
This small but powerful modifier confirms that telehealth services are treated just like in-person visits, which is crucial as telemedicine continues to grow.
Stay updated with payer guidelines, avoiding common mistakes, and keeping your documentation in order are all key steps toward billing success.
Simplify your telehealth billing with RapidClaims. By automating the application of the 95 modifier and ensuring the correct CPT codes are used, RapidClaims helps reduce errors and expedite reimbursement.
Request a Free Demo to see how RapidClaims can improve your claims process and accuracy.
FAQs
Q.1 What is the 95 modifier in telehealth billing?
The 95 modifier indicates that a telehealth service was provided through real-time, interactive audio and video technology, making it eligible for reimbursement just like an in-person visit.
Q.2 When should I use the 95 modifier?
The 95 modifier should be used when the telehealth service involves live, real-time interaction between the healthcare provider and the patient, such as a video consultation or live audio call.
Q.3 Can I use the 95 modifier for non-telehealth services?
No, the 95 modifier is only for telehealth services delivered in real-time. It should not be used for in-person visits or asynchronous communication like emails or recorded video.
Q.4 What are common mistakes when using the 95 modifier?
Common mistakes include confusing the 95 modifier with others like the GT modifier, using it for non-telehealth services, or failing to check payer guidelines for specific rules and requirements.
Q.5 What payer guidelines should I be aware of for the 95 modifier?
Different insurers, including Medicare, Medicaid, and private insurance companies, have specific guidelines for using the 95 modifier. Always check with each payer to ensure compliance with their telehealth billing requirements.
Q.6 How can RapidClaims help with telehealth billing?
RapidClaims automates the process of applying the correct modifiers and CPT codes, ensuring accuracy and reducing errors. It provides real-time suggestions for modifiers, helping healthcare providers submit claims more efficiently and improve reimbursement rates.
%201.png)