Revenue Cycle Transparency: Streamline Billing and Claims
In 2023, nearly 15% of all medical claims submitted to private insurers were initially denied, a significant increase from 9% in 2016. This surge is primarily attributed to documentation errors and inefficiencies in claim processing. For revenue cycle managers and compliance officers, these denials not only disrupt cash flow but also indicate deeper systemic issues within the revenue cycle.
The lack of transparency in tracking claims from submission to reimbursement exacerbates these challenges, leading to increased administrative costs and delayed payments. Addressing this lack of visibility is crucial for improving claim acceptance rates and operational efficiency.
This blog delves into the importance of revenue cycle transparency, exploring how enhanced visibility can streamline processes, reduce denials, and ultimately bolster financial performance.
Key Takeaways:
- Visibility Drives Performance: Limited transparency increases denials, slows A/R cycles, and raises administrative costs.
- Core Principles: Unified clinical-financial data, audit-ready processes, and patient-focused billing reduce errors and accelerate reimbursements.
- Tech-Enabled Efficiency: EHR-RCM integration, dashboards, and AI automation catch errors early and streamline workflows.
- Operational Best Practices: Standardized workflows, role-based access, and pre-submission checks improve accuracy and compliance.
- Governance & Security: Oversight, regulatory monitoring, and strong cybersecurity protect revenue and patient trust.
- Collaborative AI Tools: Solutions like RapidClaims combine AI with human oversight for real-time visibility and faster reimbursements.
Table of Contents:
- Why Revenue Cycle Transparency Matters
- Current State: What The Data Shows
- Core Principles Of Transparent Revenue Cycles
- Technology And Tools That Deliver Transparency
- Operational Practices To Improve Transparency
Governance, Compliance, And Security Considerations - Roadmap: Quick Wins And Long-Term Program Steps
Conclusion - Frequently Asked Questions (FAQs)
Why Revenue Cycle Transparency Matters
If you’ve ever wondered why claims keep getting denied or why A/R cycles stretch longer than expected, the answer often comes down to visibility. When billing, payer interactions, and patient communications aren’t fully traceable, even small gaps can slow down reimbursements and create frustration across teams.
Alt text:Why Revenue Cycle Transparency Matters
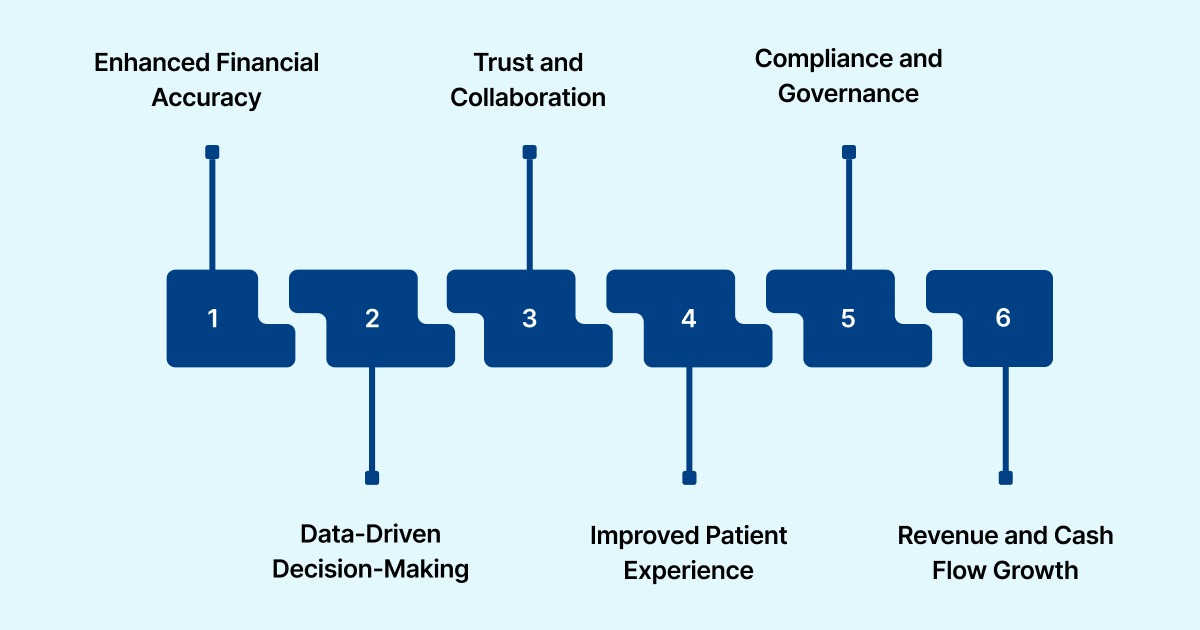
Here are the main ways transparency drives better accuracy, decisions, patient experience, and revenue:
- Enhanced Financial Accuracy: Visibility across the entire claim lifecycle reduces billing errors and denials. Organizations with transparent RCM systems report faster cash conversion cycles and quicker issue resolution.
- Data-Driven Decision-Making: Real-time insights into denials, payer delays, and claim trends allow administrators to allocate resources effectively and improve process efficiency.
- Trust and Collaboration: Shared access to claim status and reimbursement metrics strengthens coordination between clinicians, finance teams, and payers, reducing delays and compliance risks.
- Improved Patient Experience: Clear, consistent billing communication reduces confusion, financial stress, and disputes, supporting timely payments and higher patient satisfaction.
- Compliance and Governance: Transparent processes create auditable trails for all transactions, ensuring adherence to CMS and AHA standards while minimizing regulatory exposure.
- Revenue and Cash Flow Growth: Eliminating bottlenecks in coding, submission, and follow-up accelerates reimbursements, reduces bad debt, and strengthens financial resilience.
To understand the impact of transparency, let’s look at the current data and trends shaping revenue cycle performance.
Current State: What The Data Shows
Despite ongoing efforts, many healthcare organizations still grapple with transparency challenges in their revenue cycles. The following statistics shed light on the persistent issues affecting financial performance and operational efficiency.
- Improper Payments Remain High: CMS reports improper payment rates of 5.61% for Medicare Part C and 3.7% for Medicare Part D, totaling over $19 billion in avoidable spending. Medicaid and CHIP errors are mainly due to missing or insufficient documentation, not fraud, highlighting gaps in visibility.
- Administrative Inefficiency Costs: McKinsey estimates U.S. revenue cycle inefficiencies cost $200 billion per year. Each claim costs $12–$19 to process and takes 4–6 weeks to settle. Fragmented systems and limited real-time data access exacerbate delays.
- High Claim Denials: Becker’s Hospital Review (2024) found 38% of providers experience 10% or more claims denied, with 46% citing inaccurate or missing data as the leading cause. Clean claims have become harder post-pandemic due to evolving payer requirements.
- Payer-Specific Denial Rates: Private insurers deny nearly 15% of claims on average. Medicare denies 8.4%, Medicaid 16.7%, and Medicare Advantage 15.7%. Some insurers, including UnitedHealthcare and AvMed, report denial rates exceeding 30%.
- RCM Performance Benchmarks: HFMA highlights key metrics; cost to collect (3–4% of net revenue; inefficient organizations often exceed 5%) and days in A/R (cycles over 50 days indicate follow-up, posting, or denial inefficiencies).
With these challenges and patterns in mind, the next step is understanding the core principles that make a revenue cycle truly transparent.
Core Principles Of Transparent Revenue Cycles
Understanding the core principles of a transparent revenue cycle is essential for identifying hidden inefficiencies, reducing revenue loss, and improving operational clarity.
The following principles provide a roadmap for creating a revenue cycle that is reliable, accountable, and financially resilient.
1. Unified Clinical–Financial Data Visibility
Transparency begins with integrating clinical and financial data into a single, accessible system. From patient records to billing codes and insurance details, a unified view allows teams to spot discrepancies early, reduce manual rework, and prevent claim denials caused by incomplete or inaccurate data.
Accurate clinical documentation directly affects coding quality, which drives reimbursement decisions. With this visibility, stakeholders can track claim status clearly from submission to final payment, ensuring accountability across the revenue cycle.
Struggling with incomplete or inaccurate documentation affecting reimbursements? RapidCDI turns clinical notes into precise risk scores at the point of care. It improves RAF accuracy by 25%, saves physicians 25 minutes per day, boosts quality measures by 12%, and generates $2.1M in value through automated coding.
2. Explainable Processes and Auditability
Revenue cycle transparency depends on processes that are standardized, explainable, and auditable. Every step, from registration to claim adjudication, should have clear protocols and documented decision trails.
This ensures teams can quickly review, verify, and resolve errors. For example, when claims are denied, a thorough record of adjudication steps allows faster resolution. This minimizes revenue loss, and supports compliance with CMS price transparency mandates.
Also Read: Coding and Revenue Cycle Management in Healthcare: An Analysis
3. Patient-First Billing Communication
Placing patients at the center of billing communications strengthens trust and encourages timely payments. Transparent billing delivers precise cost estimates and easy-to-understand statements outlining patient responsibility. This approach reduces confusion, mitigates “sticker shock,” and increases on-time payments.
Offering flexible payment options and personalized financial guidance further enhances patient satisfaction and engagement throughout the care journey.
With these principles in place, the next step is using technology and tools that make transparency actionable across every stage of the revenue cycle
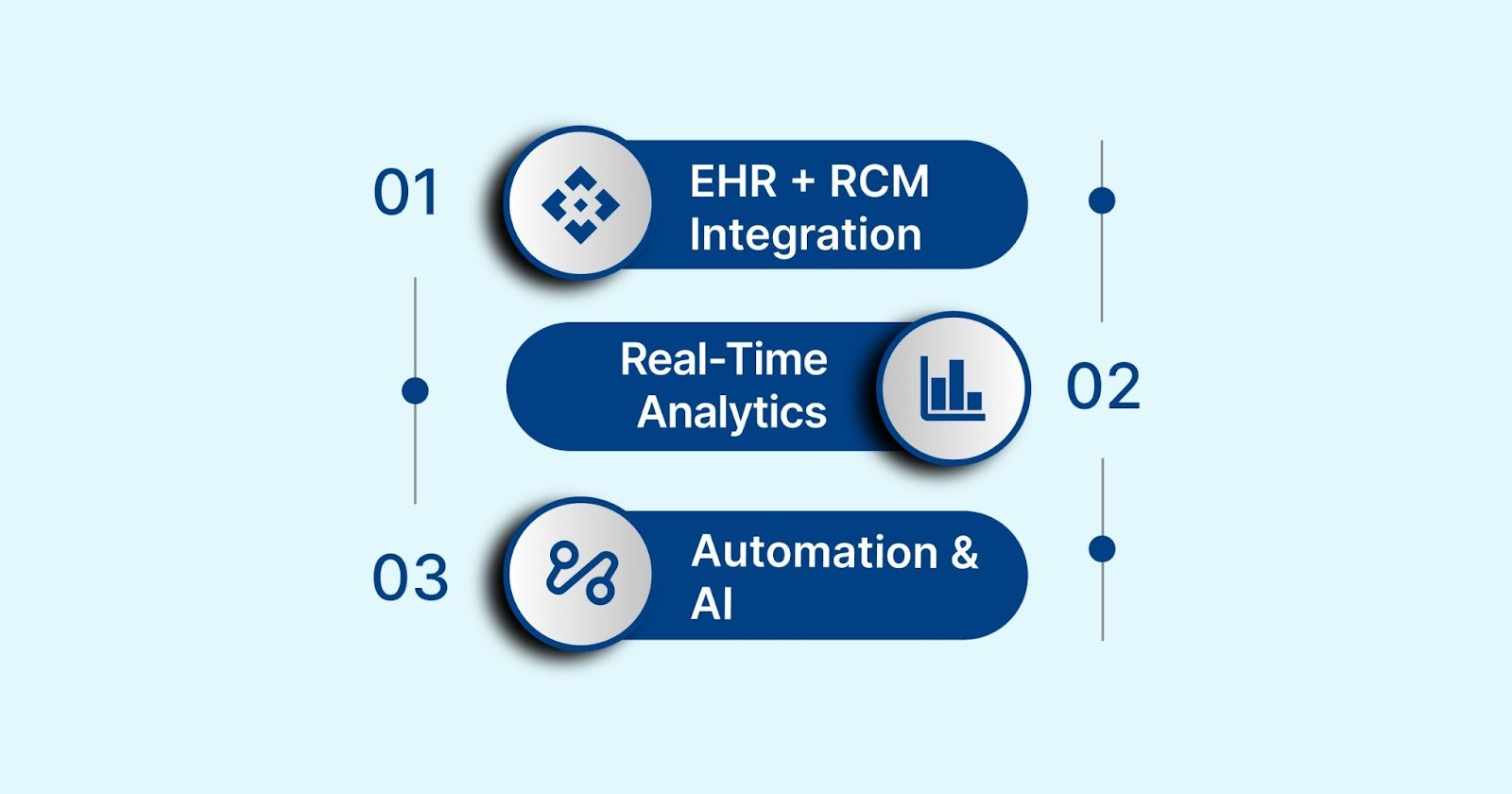
Technology And Tools That Deliver Transparency
Revenue cycle principles only work when paired with the right technology. EHR-RCM integration, real-time analytics, and AI automation give teams clear visibility into claims and billing. These tools help catch errors early, prevent revenue loss, and improve efficiency.
Alt text:Technology And Tools That Deliver Transparency
The following points explain how each tool works and the impact it delivers.
1. EHR + RCM Integration (FHIR, HL7)
EHR and RCM integration connects patient clinical records with financial and billing systems, creating a unified platform where data flows seamlessly between departments.
Why It Matters: With this integration, every encounter, diagnosis, and procedure automatically updates billing workflows. Teams can detect discrepancies immediately, track claims in real time, and reduce errors caused by manual data entry, directly lowering the risk of denials and improving revenue flow.
2. Analytics, Dashboards, and Real-Time KPIs
Advanced analytics platforms and interactive dashboards compile revenue cycle data. These present metrics such as denial reasons, days in accounts receivable, clean claim rates, and cash flow trends in a visual, digestible format.
Why It Matters: These tools allow teams to identify bottlenecks, monitor payer performance, and anticipate claim denials before they occur. By translating raw data into actionable insights, organizations can optimize workflows, make informed decisions, and strengthen overall financial control.
3. Automation & AI: From Charge Capture to Coding Validation
Automation and AI streamline repetitive revenue cycle tasks, including charge capture, eligibility verification, claim submission, and coding validation against clinical documentation.
Why It Matters: AI ensures coding accuracy, reducing denials caused by errors, while robotic process automation speeds up authorizations and payment posting. This combination decreases administrative workload, accelerates reimbursements, and provides consistent, transparent tracking of claims from submission to payment.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
Technology provides the tools, but consistent operational practices turn transparency into reliable results across the revenue cycle.
Operational Practices To Improve Transparency
Without clearly defined workflows, pre-submission checks, and patient-focused billing, even the best technology or policies cannot prevent errors or denials.

Alt text:Operational Practices To Improve Transparency
The following practices illustrate how operational rigor drives transparency and financial performance.
1. Standardized Workflows and Role-Based Access
Structured workflows define the exact steps for each revenue cycle task. Role-based access (RBAC) ensures staff only access the data relevant to their role.
Why It Matters:
- Minimizes errors and duplications.
- Protects sensitive patient and financial data.
- Supports compliance with HIPAA and payer requirements.
Example:
A coding team can access only clinical documentation and claim data, while billing staff sees insurance and payment information. This separation reduces mistakes and speeds up processing.
Structured workflows with role-based access reduce mistakes, protect sensitive data, and improve compliance. With RapidCode, teams can cut claim denials by 70%, increase coding productivity by 1.7× (saving 2 hours per day), and process over 1,000 charts per minute.
2. Pre-Submission Validation and Denial Prevention
Reviewing claims for accuracy before submission to payers. Includes verifying documentation, coding, and patient info.
Why It Matters:
- Reduces claim denials caused by missing or inaccurate information.
- Shortens reimbursement cycles.
- Protects revenue and operational performance.
Example:
Claim scrubbing software flags missing ICD codes or inconsistent patient demographics before submission, preventing denials that would otherwise require follow-ups.
High claim denials slowing you down? RapidScrub checks claims before submission, catching missing codes or mismatched patient info. It can cut denials by 70%, speed up A/R recovery by 5 days, process 1,000+ charts per minute, and reduce costs by 30%.
3. Patient Estimates, Price-Checking, and Collections Best Practices
Providing accurate cost estimates and clear billing details to patients upfront. Streamlining payment collections and offering flexible options.
Why It Matters:
- Builds patient trust and satisfaction.
- Reduces billing confusion and payment delays.
- Lowers bad debt and write-offs.
Example:
A system that calculates co-pays, deductibles, and out-of-pocket costs during scheduling allows staff to communicate total expected charges before the visit.
Operational improvements must also be supported by governance, compliance, and security measures.
Governance, Compliance, And Security Considerations
Effective governance, compliance, and security turn transparency into actionable control. Understanding these practices helps prevent revenue leakage, streamline audits, and maintain patient trust.
The following points highlight how organizations can put these measures into practice.
- Clear Governance and Roles: Assign responsibilities for each revenue cycle task. AMA data shows strong governance reduces compliance violations and improves financial outcomes.
- Monitor Regulatory Changes: Keep up with HIPAA and CMS mandates. CMS reports that proactive compliance lowers penalties and eases audits.
- Automate Compliance Checks: CMS notes that AI tools can reduce rejected claims and audits, streamlining billing and coding accuracy.
- Enhance Cybersecurity: HHS reports healthcare data breaches now cost an average of $10.93 million, highlighting the need for strong cybersecurity measures.
- Auditable Workflows: Transparent billing records simplify dispute resolution and speed reimbursement. CMS recommends defensible documentation trails.
- Integrate Clinical-Financial Systems: End-to-end visibility connects patient care and billing. McKinsey shows it improves revenue capture. Platforms like RapidClaims offer real-time insights and actionable transparency.
Also Read: Essential Guide to Healthcare Data Compliance & Protection
With governance, compliance, and security in place, the next step is mapping actionable initiatives, both immediate improvements and long-term strategies.
Roadmap: Quick Wins And Long-Term Program Steps
Revenue cycle transparency impacts both financial performance and operational clarity. Quick wins address immediate pain points like claim errors, while long-term steps ensure sustainable efficiency, compliance, and patient trust.
The table below outlines these actions for practical implementation.
Implementation Tips:
- Prioritize Based on Impact: Start with areas that have the most significant impact on revenue and compliance.
- Engage Stakeholders: Involve key personnel from clinical, financial, and IT departments in the planning and implementation phases.
- Monitor Progress: Establish key performance indicators (KPIs) to track the effectiveness of implemented strategies.
Conclusion
Achieving true revenue cycle transparency requires more than implementing isolated tools; it demands a coordinated approach that connects clinical, financial, and operational data in real time. When organizations put these practices into action, they can reduce denials, accelerate reimbursements, and strengthen overall financial resilience.
RapidClaims makes this operationally feasible, providing AI-powered solutions for coding accuracy, claim validation, and clinical documentation improvement; all integrated into your existing workflows. To see how these capabilities translate into measurable results for your team, you can book a demo and experience RapidClaims in action.
Frequently Asked Questions (FAQs)
1. What is revenue cycle transparency?
Revenue cycle transparency is the ability to track every step of the billing and claims process, from patient registration to final payment, ensuring clear visibility and accountability.
2. Why is it important for healthcare organizations?
It reduces claim denials, accelerates reimbursements, strengthens compliance, and improves both financial performance and patient trust.
3. How can AI support transparency in the revenue cycle?
AI automates claim validation, coding, and data reconciliation, helping detect errors early, prevent denials, and streamline workflows.
4. What operational practices improve transparency?
Standardized workflows, role-based access, pre-submission claim review, and clear patient billing communication are key practices.
5. How does RapidClaims help achieve revenue cycle transparency?
RapidClaims integrates AI-driven coding, pre-submission validation, and clinical documentation support, giving teams real-time visibility and reducing errors and denials.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)








