CPT And ICD Codes for Hypothalamic Obesity and Its Causes
As a medical coder or revenue cycle professional, coding rare conditions like hypothalamic obesity (HO) can be challenging. The lack of clear data and precise diagnostic criteria increases the risk of claim denials. With rare diseases, every misstep in coding can impact reimbursement.
Hypothalamic obesity is commonly linked to craniopharyngioma, a rare brain tumor affecting the hypothalamus. The annual incidence of craniopharyngioma ranges from 0.5 to 1.9 per 1,000,000 people, making HO difficult to diagnose and code accurately.
In this blog, we’ll explore the CPT and ICD codes for hypothalamic obesity and its causes. We’ll also discuss the challenges in coding this condition and provide best practices for accurate coding and documentation.
TL;DR (Key Takeaways)
- Hypothalamic obesity is caused by damage to the hypothalamus, often due to brain tumors, surgery, radiation, or trauma.
- It is resistant to lifestyle changes and requires specialized medical intervention.
- Accurate coding involves using both ICD-10-CM and CPT codes, reflecting the condition and its underlying causes.
- Key ICD-10-CM codes include those for craniopharyngiomas, brain tumors, and post-surgical or post-radiation effects.
- Correct BMI classification codes and documentation of comorbidities are crucial for accurate billing and reimbursement.
Table of Contents:
- What Is Hypothalamic Obesity?
- ICD-10-CM Coding for Hypothalamic Obesity
- Additional Obesity Classification Codes
- CPT Codes for Hypothalamic Obesity
- Genetic and Treatment-Related Causes of Hypothalamic Obesity
- Best Practices for Coding Hypothalamic Obesity
- RapidClaims: AI-Powered Solutions for Accurate Coding
- Conclusion
What Is Hypothalamic Obesity?
Hypothalamic obesity occurs when damage to the hypothalamus disrupts the brain's control over hunger, metabolism, and energy balance. This results in rapid, uncontrollable weight gain.
Common causes include:
- Brain tumors (e.g., craniopharyngiomas)
- Surgery or radiation therapy affecting the hypothalamus
- Head trauma
- Inflammatory or infectious conditions
Unlike typical obesity, hypothalamic obesity is resistant to diet and exercise, often leading to metabolic complications like insulin resistance and sleep apnea.
Basic Mechanisms of Hypothalamic Obesity
The hypothalamus regulates appetite and energy balance. Key components include:
- Arcuate Nucleus (ARC): Controls appetite and energy expenditure through AgRP/NPY neurons (stimulation) and POMC neurons (inhibition).
- Satiety Signals: Leptin and ghrelin balance hunger and fullness. Hypothalamic damage disrupts these signals, causing excessive eating and low energy expenditure.
Disruption of these pathways results in:
- Hyperphagia (excessive eating)
- Reduced energy expenditure
- Altered insulin sensitivity
This explains why hypothalamic obesity is resistant to lifestyle changes and may require medical or surgical intervention. With a clearer understanding of hypothalamic obesity, let’s now turn to how ICD-10-CM coding applies to this condition.
ICD-10-CM Coding for Hypothalamic Obesity
Accurate ICD-10-CM coding for hypothalamic obesity requires sequencing that reflects both the reason for the encounter and the causal relationship between obesity and hypothalamic dysfunction. Use class-specific obesity codes paired with adult BMI Z-codes for enhanced specificity.
Before proceeding with the correct sequence, it is important to understand how to prioritize the codes based on the focus of the encounter.
Correct Coding Sequence
1. Primary Code (Condition Chiefly Managed at the Visit):
For obesity-focused care: List E66.811 (Class 1 obesity), E66.812 (Class 2 obesity), or E66.813 (Class 3 obesity) as the primary code when the focus of the encounter is obesity management. Pair with adult BMI Z68.- codes (e.g., Z68.3–Z68.45) for added specificity.
For hypothalamic/endocrine-focused care: If the visit is primarily for managing hypothalamic dysfunction, list E23.3 (Hypothalamic dysfunction) as the primary diagnosis and the obesity code (E66.81x) as secondary.
2. Secondary Code (Underlying Cause):
E23.3 (Hypothalamic dysfunction) should be listed as the secondary diagnosis to specify the cause of the obesity. When the visit is focused on managing hypothalamic or endocrine dysfunction, list E23.3 first and the obesity class code second.
3. Tertiary Code (Specific Etiology):
Add tertiary codes for specific etiologies of hypothalamic dysfunction (e.g., D35.3 for craniopharyngioma, S06.- for TBI, Y84.2 for complications of radiation therapy, Z98.890 for postprocedural status) as supported by documentation.
Now that we’ve established the correct sequence for coding, let’s look at the specific ICD-10-CM codes that should be used for hypothalamic obesity.
ICD-10-CM Codes for Hypothalamic Obesity
Note:
Sequence codes based on the reason for the encounter:
- For obesity management, list E66.81x as the primary diagnosis and pair it with adult BMI Z68.- codes.
- For hypothalamic/endocrine management, list E23.3 first and follow with the appropriate obesity code (E66.81x).
This approach ensures accurate documentation, compliance, and reimbursement while reducing the risk of claim denials. To further enhance the accuracy of your coding, let’s take a closer look at the classification of obesity based on BMI.
Additional Obesity Classification Codes
Accurate obesity coding is essential for correct diagnosis, treatment, and reimbursement. The latest updates, effective October 1, 2024, provide clearer guidelines for classifying obesity severity using E codes and BMI Z codes for adults. Below, you will find the key codes that should be applied for proper documentation.
Obesity Severity and Class Codes (E Codes)
The E codes represent the severity of obesity, with each class based on BMI. These codes serve as the primary diagnosis and must be paired with the appropriate BMI Z codes.
Here is a breakdown of the E codes for obesity classification:
These E codes are used to document the severity of obesity in adults. They should not be paired with E66.8 ("Other obesity"). Instead, use these codes as the primary diagnosis and ensure they are paired with the corresponding BMI Z codes for additional specificity.
Adult BMI Z-Codes
In addition to E codes, the BMI Z codes provide more precise information about the patient’s BMI range. These codes should be used in conjunction with the E codes for obesity severity.
Here are the Adult BMI Z codes:
These Z codes are supplementary and should be used to specify the BMI range for adults. Ensure that the E codes for obesity severity are used as the primary diagnosis and paired with the appropriate Z68 code for the BMI range.
Key Considerations for Accurate Coding
- E66.8 ("Other Obesity"): Only use when the obesity does not fit into one of the class categories. Do not pair with E66.811–E66.813.
- E66.01 ("Morbid Obesity Due to Excess Calories"): Use only when excess caloric intake is explicitly documented as the cause of obesity. If both Class 3 obesity and morbid obesity are documented, use E66.813.
- E66.2 ("Obesity Hypoventilation Syndrome"): This code applies to obesity hypoventilation syndrome (OHS), not general breathing difficulties like obstructive sleep apnea, which should be coded separately as G47.33.
Additional Coding Tips
- BMI Z-codes: Pair Z68 codes with the appropriate E66 class code for accurate BMI documentation. Z68 should not be the primary diagnosis.
- Avoid Code Stacking: Select the most accurate obesity diagnosis (E66.-) and pair with the appropriate Z68 code.
- Stay Current: Ensure your coding team is trained on the October 1, 2024, updates and the April 1, 2025 clarification to prevent errors.
Having covered obesity classification, it’s now time to explore the CPT codes needed to bill for treatments of hypothalamic obesity.
CPT Codes for Hypothalamic Obesity
CPT codes are essential for billing services like office visits, counseling, and surgery related to hypothalamic obesity. These codes describe the services provided but do not directly define the condition itself. Always link CPT codes to the most specific ICD-10-CM codes, especially when obesity is linked to hypothalamic dysfunction, to ensure accurate billing and avoid denials.
Below is a table outlining the relevant CPT codes used in the treatment of hypothalamic obesity:
Also Read: Differences and Basics of ICD-10 and CPT Codes
Beyond the CPT and ICD codes for hypothalamic obesity and its causes, it’s essential to understand the genetic and treatment-related factors that contribute to hypothalamic obesity.
Genetic and Treatment-Related Causes of Hypothalamic Obesity
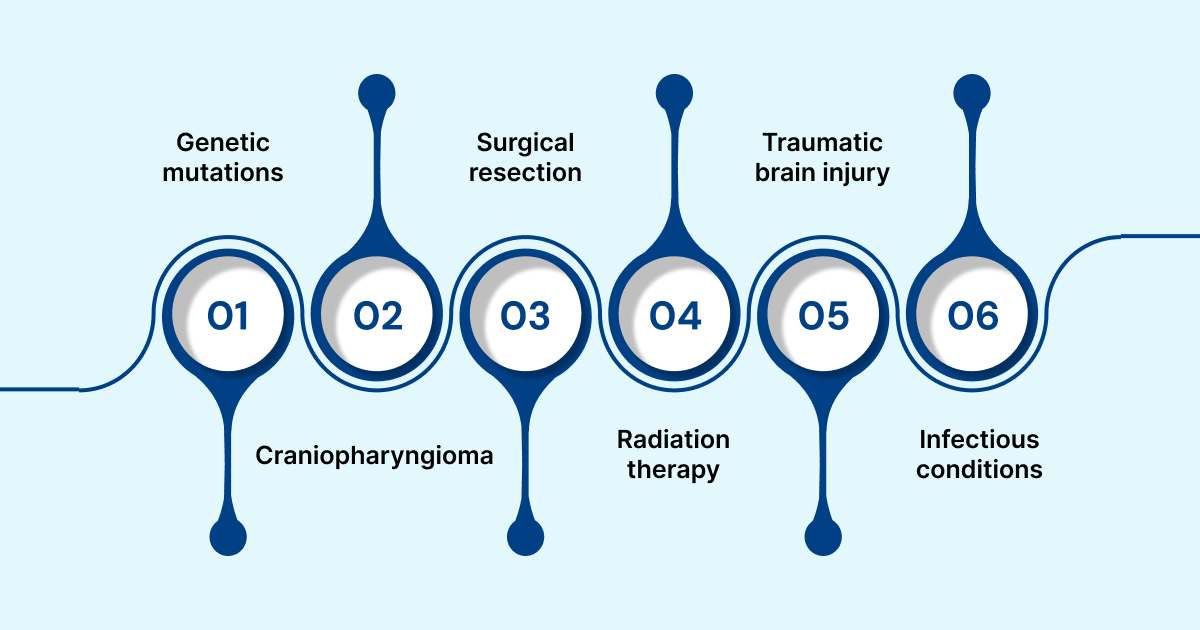
Hypothalamic obesity can result from genetic conditions or treatments that disrupt the hypothalamus, affecting appetite regulation and metabolism. Understanding these causes is key to providing the correct diagnosis and treatment. These cases often involve complex medical histories, including tumors, surgery, or genetic disorders.
Here are some common genetic and treatment-related causes of hypothalamic obesity:
- Genetic mutations (e.g., LEP, LEPR, POMC, MC4R) can disrupt the regulation of appetite and energy balance, leading to obesity.
- Craniopharyngioma is a benign brain tumor that can cause hypothalamic injury, resulting in obesity and other endocrine dysfunctions.
- Surgical resection of hypothalamic tumors can damage the hypothalamus, leading to obesity due to impaired metabolic control.
- Radiation therapy for brain tumors can cause hypothalamic damage, contributing to weight gain and other metabolic disorders.
- Traumatic brain injury affecting the hypothalamus can disrupt normal appetite regulation, leading to obesity.
- Inflammatory or infectious conditions like encephalitis or autoimmune diseases can cause hypothalamic dysfunction, resulting in obesity.
These causes are essential to document accurately for appropriate coding and treatment.
Best Practices for Coding Hypothalamic Obesity
Accurate coding for hypothalamic obesity involves following specific guidelines and practices to ensure proper billing and reimbursement. Regular updates to coding systems, along with consistent documentation practices, help prevent denials and improve the accuracy of claims.
Here are some best practices for coding hypothalamic obesity:
- Consult the ICD-10-CM Official Guidelines regularly to ensure compliance with the most up-to-date coding standards.
- Review updates from the CDC and CMS to understand any changes that could impact coding for hypothalamic obesity.
- Use professional associations, such as ACOG or the Obesity Medicine Association, for specialty-specific guidance and recommendations on coding.
- Engage in continuing education on endocrine and metabolic coding to stay current with new coding practices and procedures.
- Document the causal relationship between hypothalamic injury and obesity clearly to support the diagnosis and treatment plans.
- Include BMI Z-codes to support medical necessity for interventions and to strengthen claims for obesity-related services.
- Capture comorbidities such as type 2 diabetes or hypertension to improve risk adjustment and enhance the clinical picture.
- Verify payer-specific rules, as some insurers may require prior authorization for obesity-related counseling or nutrition therapy.
To help compliance officer and billing leads, implement these best practices, let’s look at how AI-powered solutions like RapidClaims can help revenue cycle professionals and physician group administrators improve coding accuracy.
RapidClaims: AI-Powered Solutions for Accurate Coding
RapidClaims is a B2B, enterprise-grade SaaS platform that uses AI to enhance medical coding accuracy and decrease claim denials. It automates the coding process by integrating technologies like Natural Language Processing (NLP), ensuring more precise and efficient claims management.
The RapidClaims platform is particularly useful for healthcare IT and digital transformation leaders. It helps reduce administrative workload while improving healthcare delivery, making it easier for providers to manage coding and billing tasks.
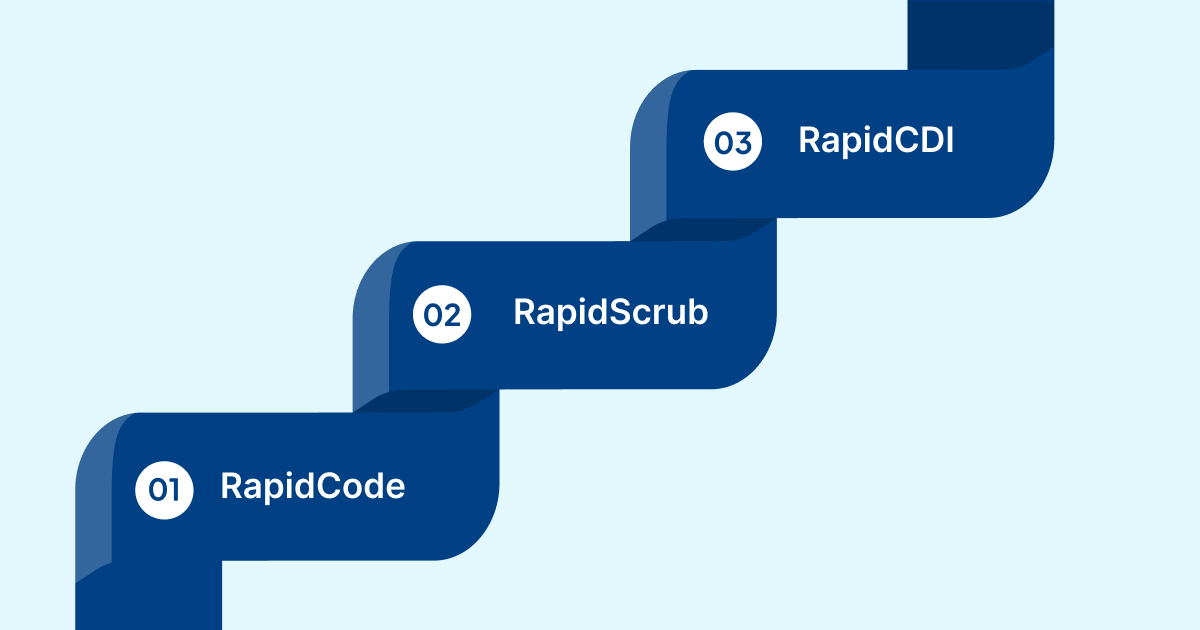
Here are the key components of RapidClaims that support accurate coding and improve coding efficiency:
- RapidCode: AI-powered medical coding system that prevents claim denials by automating code assignment and validating clinical documentation in real time.
- RapidScrub: AI-powered denial prevention tool that catches errors before submission, reducing denials and speeding up payment recovery.
- RapidCDI: A clinical documentation improvement tool that enhances coding accuracy by transforming patient data into revenue intelligence.
RapidClaims' solutions help improve risk adjustment factor (RAF) accuracy by 25%, ensuring coding reflects the true complexity of a patient's condition. They also enhance quality measures, resulting in a 15% improvement tracked through automated coding protocols. Additionally, RapidClaims saves 30 minutes per day per physician by automating routine coding tasks, significantly reducing administrative burden.
RapidClaims is designed to meet the needs of physician group administrators and healthcare providers by integrating directly with electronic health record (EHR) systems. It simplifies the coding process, allowing healthcare providers to focus more on patient care while improving reimbursement.
Conclusion
Accurate coding for hypothalamic obesity requires careful attention to detail and a clear understanding of its underlying causes. With tools like Rapidclaims' AI-powered solutions, RapidCode, medical coding accuracy improves significantly, reducing claim denials and administrative burden.
For healthcare providers aiming to enhance revenue cycle management, integrating RapidScrub with HL7/FHIR-enabled EHR systems helps detect errors early and recover lost revenue. RapidCDI turns coding and clinical data into actionable insights, ensuring faster, more accurate reimbursement while maintaining compliance with industry standards.
Contact us today to learn how automation in RCM can streamline your coding process and improve reimbursement.
FAQs
1. What are the primary causes of hypothalamic obesity?
Hypothalamic obesity is caused by damage to the hypothalamus from brain tumors (e.g., craniopharyngiomas), surgery, radiation, head trauma, or infections like encephalitis. Less common causes include autoimmune disorders, vascular issues, and congenital conditions like Prader–Willi syndrome.
2. How do I correctly code hypothalamic obesity in ICD-10?
Use E66.811–E66.813 based on BMI class, paired with E23.3 for hypothalamic dysfunction. Add adult BMI Z68.- codes when documented. Sequence by encounter focus: obesity management first, then hypothalamic dysfunction.
3. Which ICD-10 code should be used for obesity caused by hypothalamic dysfunction?
Use E66.811–E66.813 based on the documented obesity class, paired with E23.3 for hypothalamic dysfunction. Include adult BMI Z68.- codes if documented.
4. What is the ICD-10 code for hypothalamic amenorrhea?
Code the type of amenorrhea, such as N91.1 (Secondary amenorrhea), and add E23.3 for hypothalamic dysfunction. If documentation supports "functional hypothalamic amenorrhea," E28.39 (Other ovarian dysfunction) can be used, but it’s not required.
5. Are there specific ICD-10 codes for different classes of obesity?
Yes, obesity is classified under E66 in ICD-10 with codes for each class based on BMI: E66.811 for Class 1 obesity (BMI 30.0–34.9), E66.812 for Class 2 obesity (BMI 35.0–39.9), and E66.813 for Class 3 obesity (BMI ≥40). These should be paired with the corresponding Z68.- codes for precise BMI documentation.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






