.webp)
An Introduction to AI for Medical Coders


Medical coding is a complex field that demands high accuracy and attention to detail. With staff shortages and constant regulatory changes, it's easy for teams to feel stretched thin. This often leads to errors that can disrupt the entire billing cycle. In fact, denied claims surpassed 450 million in 2024, creating a $19.7 billion burden for hospitals to overturn.
AI addresses these challenges by automating routine tasks and helping your team manage growing workloads and stay current with constant regulatory changes. They act as an extension of your expertise, ensuring every claim is clean and compliant.
This article is an introduction to AI for medical coders. We'll break down how this technology works, its core benefits, and how it can assist your team in creating a more efficient and accurate revenue cycle.
Key Takeaways
- Challenge of Traditional Coding: Manual processes often lead to errors, delays, and financial strain due to heavy workloads and constant regulatory changes.
- Core AI Functionality: AI utilizes Natural Language Processing (NLP) and Machine Learning (ML) to interpret clinical documentation, automate code suggestions, and proactively detect errors.
- Primary Benefits: The technology dramatically increases coding accuracy and operational efficiency, directly leading to a faster revenue cycle and enhanced regulatory compliance.
- Evolving Coder Role: The job is shifting from routine data entry to quality control, specialized auditing, and mastering complex cases that require human judgment.
- A Collaborative Tool: Despite limitations in context and nuance, AI serves as a powerful, collaborative tool that significantly improves the entire healthcare finance workflow.
Table of Contents:
- The Challenges of Traditional Coding
- How AI Works for Medical Coders
- The Benefits of AI for Medical Coding
- Limitations of Using AI for Medical Coding
- The Evolving Role of a Medical Coder
- The Future of AI in Medical Coding
- Conclusion
- FAQs
The Challenges of Traditional Coding
Medical coding involves accurately translating thousands of complex medical records into codes for billing. This manual process often presents significant difficulties, which can affect a healthcare organization's finances and operations.
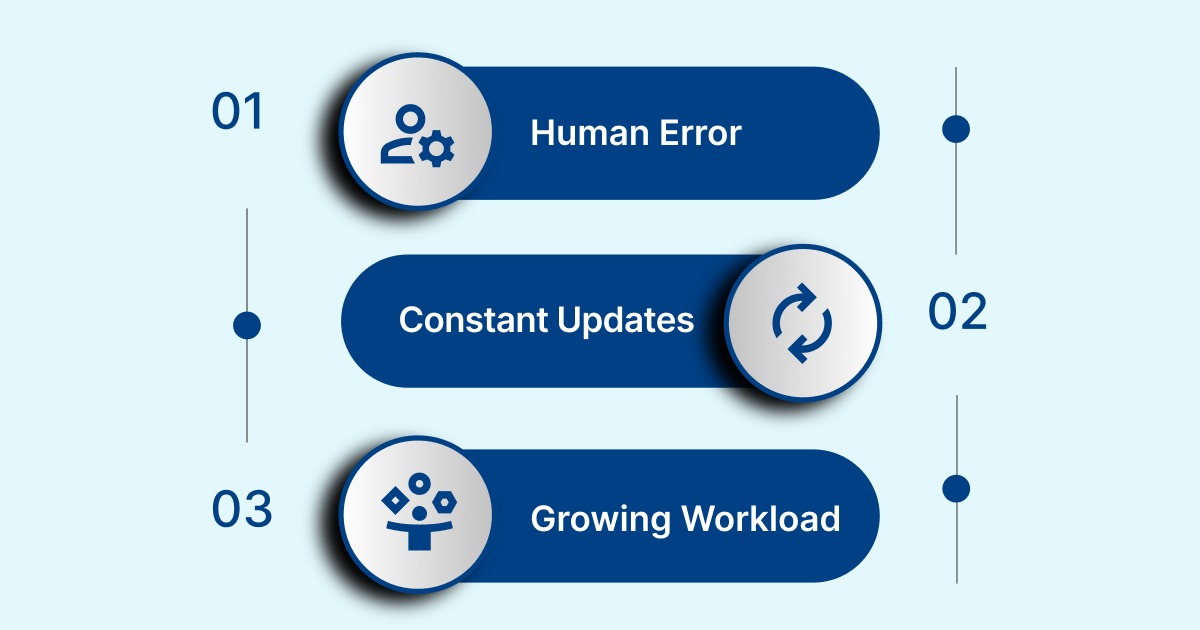
Here are some of the main challenges faced by medical coders:
- Human Error: A single typo or a misunderstood note can lead to a rejected claim, causing payment delays or even lost revenue.
- Constant Updates: Coding systems are frequently updated with new rules and codes. Staying current requires ongoing training and a lot of time.
- Growing Workload: As patient visits increase, so does the volume of records. The sheer amount of work can create a backlog, putting pressure on coders.
AI for medical coders is a powerful tool designed to support human professionals. It analyzes patient documentation and quickly suggests the correct codes. This technology helps eliminate errors and handles the routine parts of the job, allowing coders to apply their knowledge to more complex cases.
With an AI-powered tool like RapidCode, medical coders can instantly get highly accurate code suggestions from a single, easy-to-use platform, ensuring every claim is clean.
But how does this technology actually work?
How AI Works for Medical Coders
AI is a combination of advanced technologies that process vast amounts of data to provide intelligent assistance. Let’s look at the core technologies that enable AI and the practical functions they perform to support medical coding.
The Technology Behind the Process
The intelligence of an AI-powered coding system comes from its ability to process, understand, and learn from a variety of data sources. These are the key technologies that make it all possible.
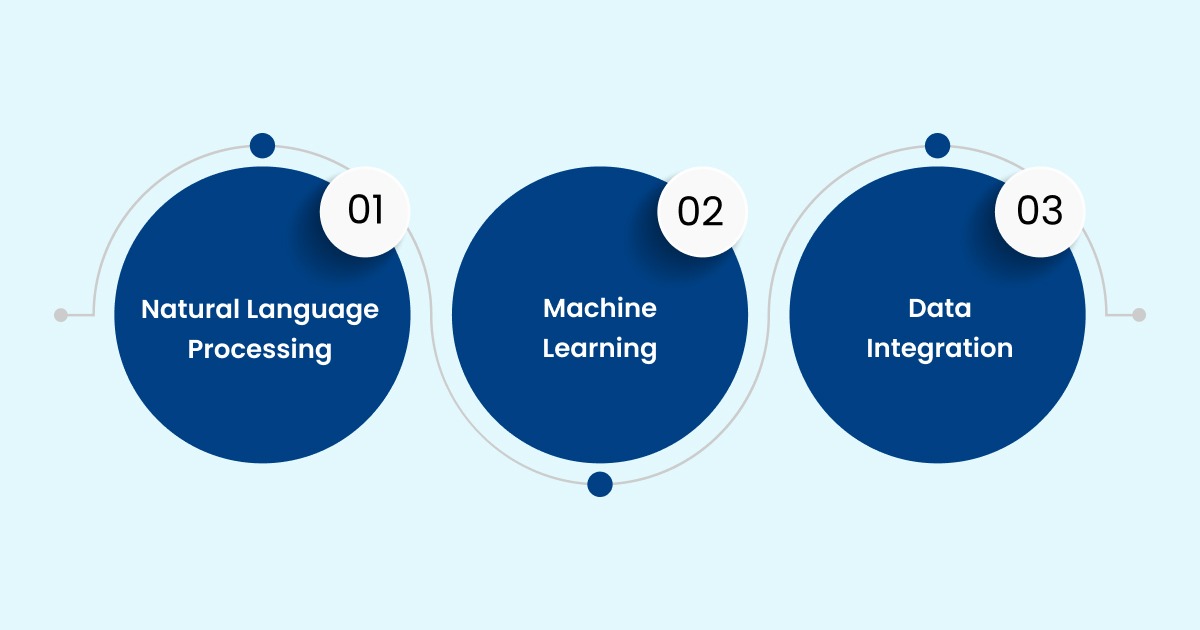
- Natural Language Processing (NLP): This foundational technology allows the AI to read and interpret unstructured clinical text, such as a physician's notes. It's how the system "understands" the meaning behind medical narratives, translating human language into a format the computer can use.
- Machine Learning (ML): Once the AI can understand text via NLP, machine learning algorithms enable it to learn from experience. By analyzing millions of past records, the system identifies patterns between documentation and appropriate codes, constantly improving its accuracy and adapting to new information.
- Data Integration: An AI system requires access to a complete view of a patient's visit. Data integration ensures that the AI can connect to various sources, such as the Electronic Health Record (EHR) and billing system, to gather all necessary information, from a lab result to a physician's note, for accurate suggestions.
Also Read: Top 10 Medical Billing Companies in USA
Key Functions of AI in Coding
Building on the foundation of the technologies above, AI systems perform specific functions that directly assist medical coders in their daily work.
- Automated Code Suggestion: Instead of a manual search, the AI analyzes a patient's chart and generates a list of relevant codes. These suggestions often include a confidence score, giving the coder a valuable starting point for their review.
- Error Detection: AI can quickly cross-refer codes with the patient's documentation to flag potential errors, such as a diagnosis code that doesn't match the procedure code or a missing modifier. This helps catch inconsistencies before a claim is submitted, reducing costly denials and audits.
With a solution like RapidScrub, teams can identify and fix errors with precision before a claim is ever sent.
- Pattern Recognition: Beyond single charts, AI can analyze trends across an entire organization's data. For example, it can identify if a particular provider consistently under-documents a certain condition, providing actionable insights to improve overall coding practices.
With a clear understanding of the technology, it is important to see the tangible benefits these systems provide.
The Benefits of AI for Medical Coding
AI solutions enhance human capabilities, acting as a reliable partner for medical coding professionals. By automating complex tasks, AI enables coders to work more efficiently and accurately.
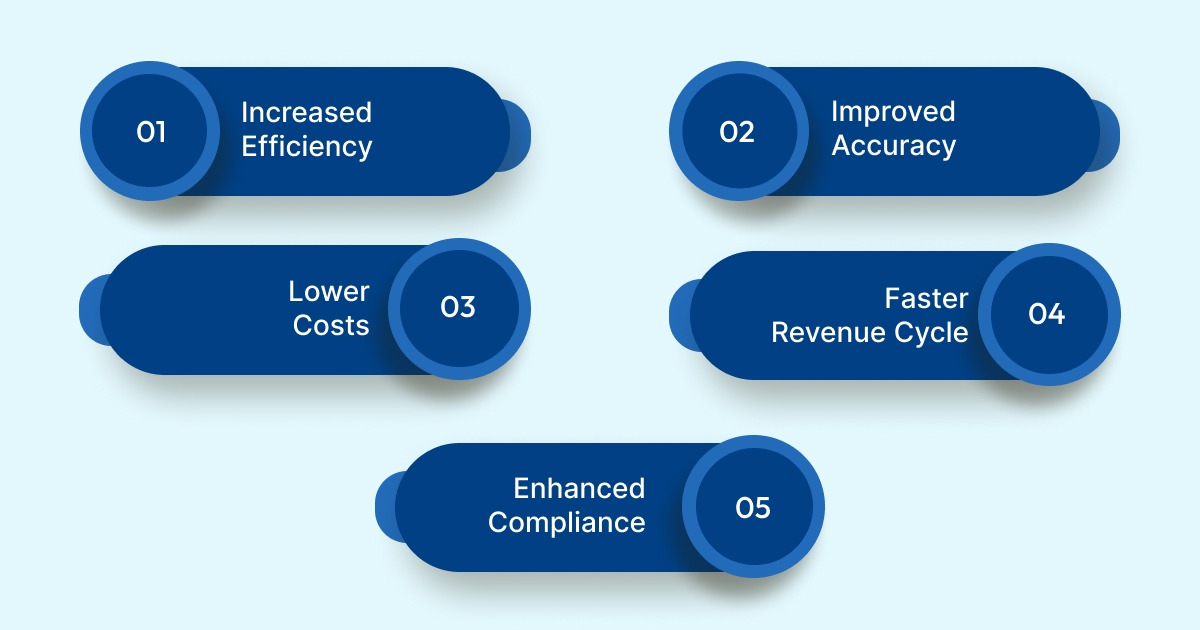
Here are some of the key advantages for coders and healthcare organizations:
- Increased Efficiency: By automating repetitive, high-volume tasks, AI frees up a coder’s time for more complex cases that require human judgment. This AI-powered automation can dramatically reduce the time spent on chart reviews and code selection. As a result, coders can handle a higher volume of work and focus their expertise where it is most needed.
- Improved Accuracy: AI systems are designed to minimize human error by consistently applying the latest coding guidelines. They can cross-reference patient documentation with millions of data points, ensuring codes are correctly assigned and reducing inconsistencies. This level of precision leads to cleaner claims and fewer errors that could result in denials or costly audits.
- Lower Costs: The financial impact of AI is significant, as it helps reduce expenses in several areas. Organizations can reduce the need for expensive contract coders and minimize costly claim denials. By making the entire coding workflow efficient, AI drives operational savings that directly contribute to the bottom line.
- Faster Revenue Cycle: The speed and accuracy of AI directly accelerates the billing process. By catching errors before claims are submitted, AI-powered systems reduce the rate of denials and the time spent on rework. This results in quicker payments, improving the financial health of the organization.
- Enhanced Compliance: The ever-changing nature of coding guidelines and regulations can make compliance a challenge. AI provides an advantage by continuously monitoring and applying the latest updates. This helps ensure that every code is compliant with current industry standards, significantly lowering the risk of fines and legal penalties.
However, it's also crucial to understand the limitations of AI and why human oversight remains essential.
Also Read: Common Types and Usage of Medical Coding Examples
Limitations of Using AI for Medical Coding
While AI offers significant potential, its application in medical coding faces several key limitations and challenges that require human oversight and strategic planning. These challenges are primarily centered on data, technology, and integration.
- Data and Quality Concerns: A major limitation is the reliance on high-quality, unbiased training data. If the data used to train the AI models is incomplete, inconsistent, or reflects historical biases (e.g., underrepresentation of certain patient demographics), the AI's output will be flawed. This can lead to inaccurate coding and potential health disparities.
- Context and Nuance: AI systems can struggle with the complexity and ambiguity of medical documentation. Unlike a human coder, an AI may not fully grasp the context of a patient's entire medical history, nor can it account for subtle nuances in a physician's notes or the social factors that influence care.
- Integration with Existing Systems: Integrating new AI-powered solutions with a healthcare provider's existing electronic health record (EHR) and billing systems can be a significant technical and financial challenge. Many legacy systems are not designed to work together easily, creating data silos and workflow disruptions.
- "Black Box" Problem and Explainability: For many advanced AI models, it is difficult to understand the reasoning behind their output. This "black box" problem creates a barrier to trust and accountability, as it is crucial for human coders to be able to justify and audit the codes assigned to ensure compliance and prevent claim denials.
These limitations highlight why the human role is not being replaced but is, in fact, evolving into something more valuable and strategic.
The Evolving Role of a Medical Coder
In an AI-driven future, the medical coder's role is not replaced but rather elevated. AI handles the routine, high-volume tasks, freeing up coders to focus on the more complex and valuable aspects of the job. This partnership allows human expertise to overcome the limitations of AI.

- Applying Human Judgment and Clinical Context: While AI can process vast amounts of data, it cannot exercise clinical judgment. Coders are essential for interpreting ambiguous documentation, understanding the full patient context, and applying their experience to make ethical and accurate decisions.
- Mastering Complex Cases: AI systems are well-suited for straightforward cases. However, complex procedures, cases with multiple co-morbidities, or rare diagnoses require the nuanced understanding of a human professional. Coders can handle the gray areas of documentation that an AI might miss, ensuring accurate and compliant coding.
- Auditing and Quality Control: Coders will transition into roles as AI auditors and validators. They will be responsible for reviewing the codes suggested by AI systems to ensure accuracy and compliance. This human oversight is crucial for preventing errors, reducing claim denials, and maintaining the financial integrity of a healthcare organization.
- Transitioning into Specialized Roles: With AI handling the basics, coders can specialize in Clinical Documentation Integrity (CDI). They can work to improve the quality of patient records, a task made simpler with an AI-powered solution like RapidCDI. Other roles include data analysts who use AI insights to optimize the revenue cycle, and compliance officers who ensure the organization follows all regulations.
Looking ahead, the next phase of this transformation promises even more intelligent and integrated solutions.
The Future of AI in Medical Coding
The integration of AI is poised to fundamentally transform medical coding, with employees globally anticipating a positive career impact. This aligns with recent data showing that more than half (52%) of workers expect AI to increase their productivity and efficiency. The future will see a shift toward more predictive, integrated, and efficient systems.
- Predictive Analytics: AI will move beyond coding to predict potential errors and revenue issues before they happen, preventing claim denials and optimizing revenue.
- Smooth EHR Integration: AI will be built directly into Electronic Health Records (EHRs), providing real-time coding suggestions as physicians document care. This reduces administrative burden at the point of care.
- Generative AI for Documentation: Generative AI will automatically summarize complex patient narratives and flag incomplete information, ensuring all necessary data is captured for accurate billing.
Also Read: Becoming a Medical Coding and Billing Specialist: Steps to Get Certified
Conclusion
The future of medical coding relies on the collaborative power of professionals and AI. Instead of replacing human expertise, AI handles routine and repetitive tasks, allowing medical coders to focus on the complex cases that require their judgment. This change improves accuracy and efficiency, and strengthens the role of the medical coder.
This new era, where human skill and technology work together, defines the future of healthcare finance. To improve your operations, you'll need a reliable partner. RapidClaims helps you manage your revenue cycle with an automated solution.
Request a demo from RapidClaims today for a smarter approach to medical coding.
FAQs
1. Will AI replace medical coders?
No. Instead of replacing coders, AI handles the repetitive, high-volume tasks. This allows human professionals to focus on complex cases that require their judgment, clinical knowledge, and problem-solving skills, elevating their role from data entry to quality assurance and auditing.
2. How does an AI solution handle new or unusual medical codes?
An AI solution uses machine learning algorithms to continuously learn from new data, including coding updates and regulatory changes. However, for genuinely new or complex cases, the AI will provide a confidence score and flag the record for a human coder to review and make the final decision.
3. What kind of training is needed for a team to adopt an AI coding solution?
Initial training typically focuses on understanding the new workflow, learning how to interpret AI’s suggestions, and using the dashboard to identify and resolve errors. For coders transitioning into new roles, additional training may be needed in areas like clinical documentation improvement (CDI) or data analysis.
4. Is AI for medical coding HIPAA-compliant and secure?
Yes. Any reputable AI solution for medical coding must be designed with strict adherence to HIPAA and other data privacy regulations. This includes using secure data encryption, robust access controls, and de-identifying data during the training process to protect patient information.
%201.png)