Why Autonomous Coding is Essential For Medical Billing
The Global Autonomous Medical Coding Market was valued at USD 2.34 billion in 2023 and is projected to more than double by the end of 2030. This shift reflects the increasing demand for automation in healthcare. Medical coders and revenue cycle managers face mounting pressure to improve accuracy while reducing costs and errors.
Medical coding has long been a complex and time-consuming task, often leading to costly mistakes. With rising demands for accuracy and compliance, compliance officers and billing leads of healthcare organizations are turning to new technologies to solve these issues. The challenge is clear: how to meet these needs while staying within budget.
In this blog, we’ll explore autonomous coding in medical billing, comparing it to traditional methods, discussing key technologies, and evaluating its benefits and challenges. We will also help you choose the right solution for your organization.
TL;DR
- AI Adoption in Coding: Autonomous coding uses AI to automate the medical coding process, reducing human involvement and increasing speed.
- Key Technologies: Machine learning, natural language processing, and predictive analytics power autonomous coding systems.
- Human Coders' Role: Coders focus on oversight, review of complex cases, and ensuring compliance, while automation handles routine tasks.
- Challenges: Automated coding faces issues with ambiguous documentation, integration complexities, and the need for human validation in complex cases.
- Future Outlook: AI will continue to improve coding accuracy, integrate with more systems, and assist coders in high-level decision-making.
What Is Autonomous Coding?
Autonomous coding refers to the use of AI technology to automatically assign medical codes, minimizing the need for human intervention. It improves speed, accuracy, and compliance by analyzing patient data and documentation on its own. This solution is designed to lighten the load for coders while maintaining high standards in medical coding.
To better understand how autonomous coding works, it's essential to look at the technologies behind the scenes.
Key Technologies in Autonomous Coding
Autonomous coding relies on several advanced technologies to function efficiently and accurately. These technologies enable automated coding systems to process clinical data, make accurate decisions, and ensure that coding practices meet regulatory standards.
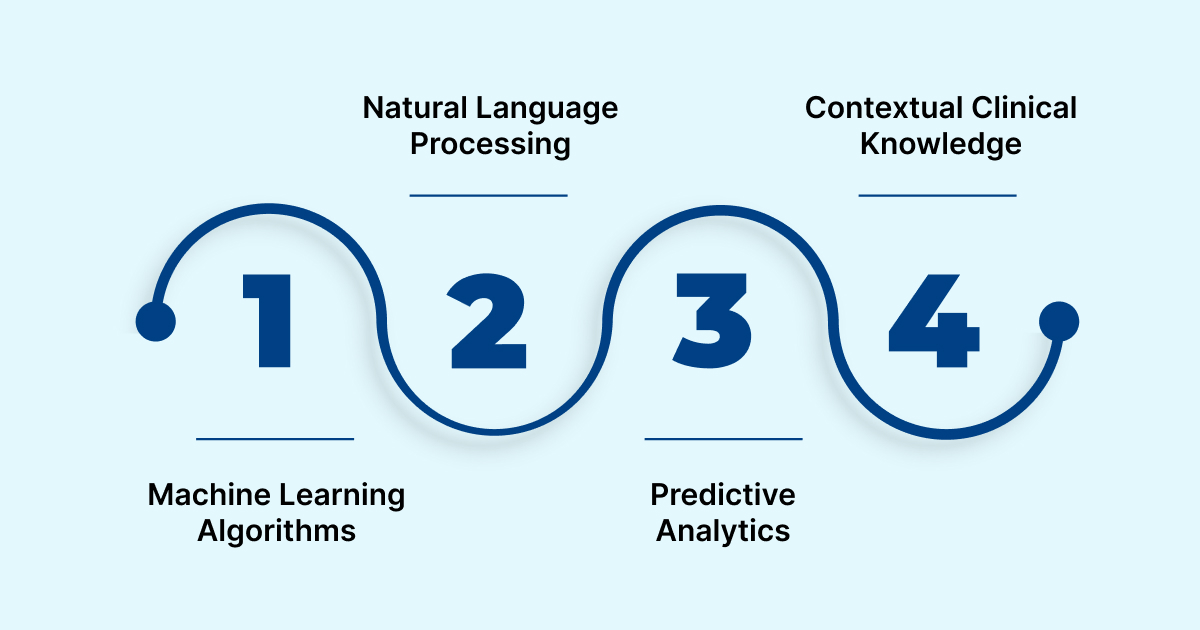
Here are the key technologies involved in autonomous coding:
- Machine Learning Algorithms: These algorithms learn from data, enabling AI to predict and assign correct codes for diagnoses and procedures.
- Natural Language Processing (NLP): NLP helps AI interpret unstructured clinical text and convert it into structured coding data.
- Predictive Analytics: Predictive analytics spot patterns in coding data, helping to identify errors or inconsistencies before they become issues.
- Contextual Clinical Knowledge: AI systems use medical knowledge databases to understand complex clinical terms and assign the most accurate codes.
Now, let’s look at how autonomous medical coding compares with computer-assisted coding (CAC) to better understand the distinctions and benefits.
Autonomous Coding vs. Computer-Assisted Coding (CAC)
Autonomous coding and computer-assisted coding (CAC) both aim to improve coding accuracy and efficiency, but they differ in the level of human involvement and the degree of automation.
Now that we know the differences, let’s take a closer look at the process of how autonomous coding is executed.
How Does Autonomous Coding Work?
Autonomous coding relies on AI technologies to automatically analyze and assign medical codes based on patient data and clinical documentation. It reduces human involvement and increases both speed and accuracy by processing large volumes of medical information.
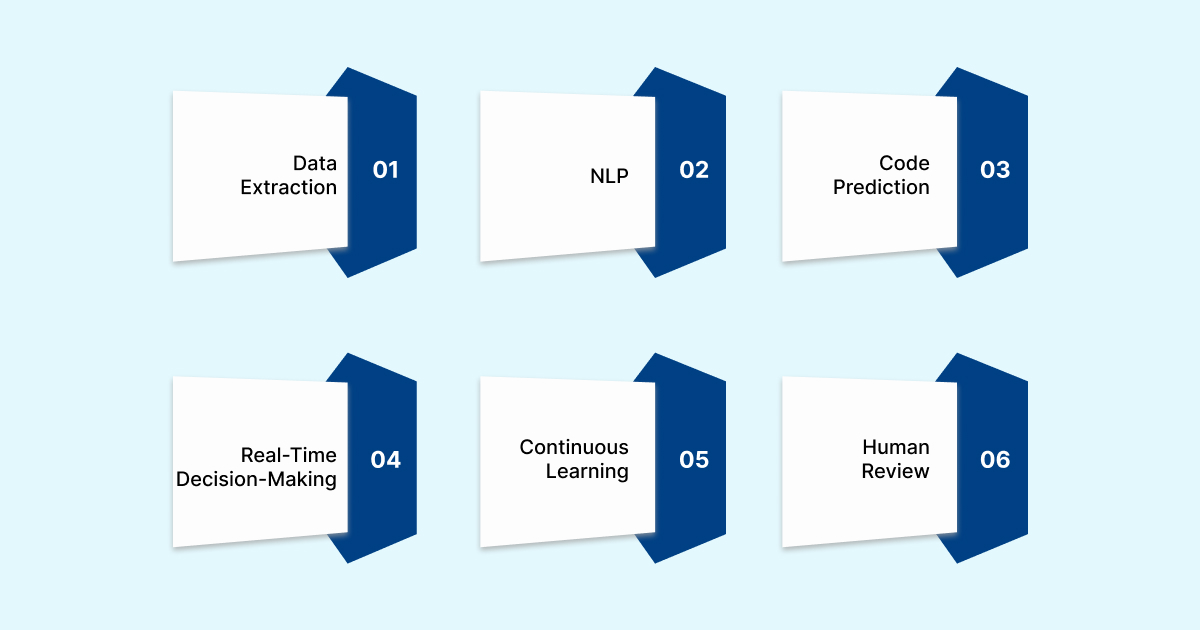
Autonomous coding systems are trained to handle complex clinical scenarios and ensure coding compliance. Here’s how autonomous coding works:
- Data Extraction: The system extracts relevant patient information from electronic health records (EHR) and clinical documentation.
- Natural Language Processing: NLP interprets unstructured clinical text, such as physician notes, to identify critical details needed for accurate code assignment.
- Code Prediction: Machine learning models predict the most appropriate codes by analyzing patterns from historical data and vast medical databases.
- Real-time Decision-making: The AI system continuously applies coding rules and guidelines in real time to ensure compliance and accuracy.
- Continuous Learning: As the system processes more data, it refines its algorithms, improving coding accuracy and adapting to changing coding standards.
- Human Review: While AI handles the bulk of coding, a coder may review complex cases, ensuring high accuracy and regulatory compliance.
While AI handles much of the work, human coders still play a key role in the coding process. Let’s explore their involvement.
RapidCode by RapidClaims offers an AI-powered solution to enhance coding accuracy and speed. With minimal setup time, it integrates seamlessly into your existing workflows. Start automating your coding today for faster reimbursements and fewer denials.
The Role of Human Coders in an Autonomous System
AI systems handle the majority of the coding tasks, but human oversight ensures that complex cases are accurately processed. Coders contribute by reviewing AI-generated code and making adjustments when needed.
Here’s how human coders fit into an autonomous coding system:
- Quality Control: Coders review AI-assigned codes for accuracy and ensure they align with the latest coding standards and regulations.
- Complex Case Handling: For complex or unclear cases, human coders apply their expertise to verify or correct AI-generated codes.
- Regulatory Compliance: Coders ensure that AI-generated codes meet all compliance requirements and address any potential issues flagged by the AI system.
- Continuous Learning: Coders contribute to AI training by providing feedback on errors or inconsistencies in AI's coding decisions, helping to improve the system’s performance.
- Collaboration: Coders collaborate with AI tools, enhancing their efficiency and reducing their workload while maintaining control over the final coding decisions.
Understanding the coder’s role helps us appreciate the benefits that autonomous coding brings to the table.
Key Advantages of Autonomous Coding in Healthcare
Autonomous coding offers several key benefits for healthcare organizations, including improved accuracy, reduced costs, and better compliance with regulations. By automating the bulk of the coding process, AI helps coders focus on more complex tasks. These benefits make it an essential tool for modern healthcare operations.
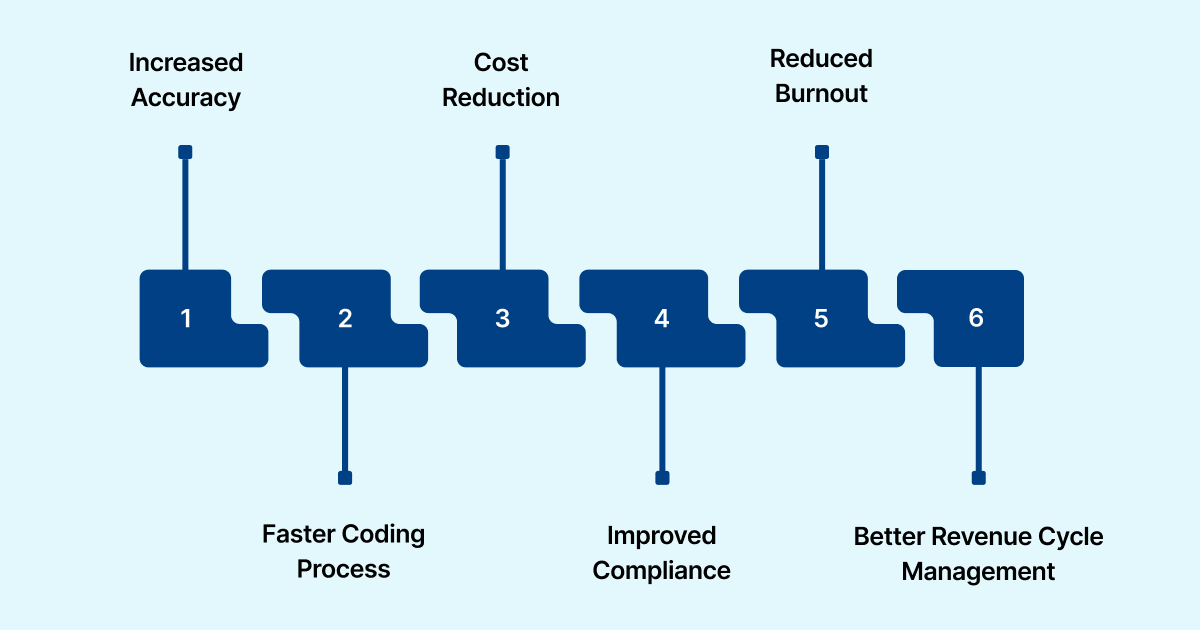
Here are the primary benefits of autonomous coding:
- Increased Accuracy: AI reduces human error by processing data consistently and following coding guidelines, ensuring accurate code assignment.
- Faster Coding Process: AI speeds up the coding process, allowing coders to complete tasks more quickly and submit claims faster.
- Cost Reduction: By reducing the time spent on manual coding, organizations can save on operational costs and increase overall productivity.
- Improved Compliance: AI systems stay up-to-date with the latest coding guidelines and regulatory changes, ensuring consistent compliance.
- Reduced Burnout: By automating repetitive tasks, coders can focus on more complex and interesting work, helping to reduce stress and improve job satisfaction.
- Better Revenue Cycle Management: Autonomous coding improves claim accuracy, which leads to fewer rejections and delays, resulting in a more efficient revenue cycle.
With RapidScrub, prevent claim denials before they happen. Our AI-powered solution quickly detects errors and optimizes your claims, ensuring faster approvals and improved cash flow. Start today and reduce your denial rates.
While there are many advantages to autonomous coding, it's also important to recognize the challenges that may arise.
Potential Pitfalls of Autonomous Coding in Healthcare
Medical coding requires a deep understanding of medical terminology, with ICD-10 containing around 68,000 diagnosis codes. As these codes and coding guidelines are regularly updated, maintaining accuracy becomes more challenging, especially with the use of autonomous coding systems.
Here are some more challenges of autonomous coding:
- Technological Limitations: Automation systems can struggle with ambiguous or incomplete clinical documentation, leading to incorrect code assignment.
- Data Quality: The accuracy of autonomous coding depends on the quality of the data input into the system, which may vary.
- Human Oversight: Despite automation, human coders are still necessary to review complex cases and correct AI mistakes when needed.
- Integration Issues: Integrating autonomation systems with existing EHR platforms and other healthcare software can be time-consuming and costly.
- Training Requirements: Coders must be trained to work alongside AI systems, understanding how to provide feedback and adjust coding when necessary.
- Cost of Adoption: Although autonomous coding can save money over time, the initial costs for technology and training can be quite high.
Understanding the challenges involved allows you to make a well-informed choice when selecting an AI solution vendor for medical coding.
Selecting the Right Autonomous Coding Vendor
Selecting the right autonomous coding vendor is key to ensuring the successful adoption of AI in medical coding. The best solution should improve accuracy, reduce manual effort, and align with your organization’s goals. Each vendor offers unique capabilities, so choosing one that fits your workflow is essential.
Here are the key factors to consider when selecting a vendor:
- System Compatibility: Choose a vendor whose software connects smoothly with your current EHR and billing systems without disrupting daily operations.
- AI Accuracy: Verify that their AI models are trained with large datasets and deliver consistent accuracy across diverse coding scenarios.
- Regulatory Compliance: Confirm the system stays current with coding standards and meets compliance requirements across ICD, CPT, and HCPCS codes.
- Speed and Performance: Select a solution that processes data quickly and maintains accuracy even with high chart volumes.
- Customization: Look for flexibility in adapting workflows, specialty-specific rules, and custom reporting features.
- Training and Support: The vendor should provide clear training, responsive technical support, and regular system updates to ensure sustained performance.
A trusted choice is RapidClaims RapidCode, designed to fit directly into your setup with zero setup delays. It reduces claim denials by 70%, improves coder productivity by 1.7x, and processes over 1,000 charts per minute. With transparent audit trails and intelligent E&M analysis, it delivers accuracy and compliance for every claim.
The Future of Autonomous Coding
The next era of medical coding will be driven by deeper integration of AI systems with clinical documentation and coding workflows. Automation is likely to handle high-volume coding tasks while human coders focus on audits, complex cases, and strategic oversight.

Here are key trends shaping the future of autonomous coding:
- EHR and data interoperability: AI coding systems will gain improved access to clinical and administrative data across platforms, enhancing accuracy, as seen in RapidCode, which ensures easy integration with existing healthcare systems.
- Predictive analytics for coding patterns: Systems will anticipate likely codes based on clinical context, reducing errors and claim rejections, a feature empowered by tools like RapidScrub for denial prevention and recovery.
- Human-AI collaboration models: Coders will shift roles toward oversight, quality review, and exception management rather than manual code entry.
- Global standardization and guideline compliance: AI tools will adapt more rapidly to coding standards across regions and specialties, improving consistency, helping tools like RapidCDI in transforming data into actionable revenue intelligence.
- Ethics, transparency and auditability: AI systems in coding will be designed for explainability, traceability and fairness to meet regulatory and organizational standards.
For healthcare providers and coding professionals, these trends represent an opportunity to build a more accurate and accountable medical coding process powered by both human and artificial intelligence.
Conclusion
Autonomous coding is changing how medical billing companies and physician group administrators manage accuracy, compliance, and revenue cycles. It reduces manual workload, minimizes claim denials, and allows coders to focus on higher-value work. With the right AI solution, healthcare teams can achieve faster reimbursements, stronger compliance, and improved productivity.
Choosing the right technology partner makes all the difference. RapidClaims delivers AI-driven medical coding that prevents denials, accelerates reimbursements, and helps your team focus on patient care.
Try RapidClaims today to experience faster, smarter medical coding built for accuracy, compliance, and measurable results.
FAQs
1. Can medical coding be done by AI?
Yes, AI can handle much of the coding process, particularly high-volume tasks, by analyzing patient data and assigning appropriate codes. However, human oversight is still needed for complex cases and regulatory compliance.
2. Can automated coding replace a coder?
AI can automate many aspects of medical coding, but it is unlikely to completely replace coders. Coders will continue to play a critical role in reviewing complex cases and ensuring compliance with coding standards.
3. What are the four types of medical coding?
The four main types of medical coding are ICD, CPT, HCPCS, and ICD-10-PCS. Each is used for different purposes, like coding diagnoses, procedures, and services. These systems ensure accurate cloud-based billing and compliance.
4. What does autonomous mean in coding?
In coding, "autonomous" refers to AI systems that perform coding tasks independently without direct human input. These systems analyze clinical data and assign codes based on learned patterns.
5. How does autonomous coding improve revenue cycle management?
Autonomous coding speeds up the coding process, reduces errors, and ensures compliance, leading to fewer claim denials and faster reimbursements. This results in more efficient revenue cycle management and improved cash flow.
.png)
Mounika L
Mounika L is a skilled medical coder with 2 years of E/M Outpatient experience, specializing in accurate CPT, ICD-10, and HCPCS coding to ensure compliance and optimize reimbursement outcomes at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






