.webp)
Understanding Ambulatory Payment Classification (APC)


Outpatient services account for a growing share of healthcare delivery, and with that growth comes the need for accurate, timely reimbursement. For providers participating in Medicare’s Outpatient Prospective Payment System (OPPS), Ambulatory Payment Classifications (APCs) are central to how outpatient care is categorized, coded, and ultimately paid for.
Despite their importance, APCs can be complex to navigate. From keeping up with regulatory changes to ensuring coding accuracy and proper documentation, even experienced billing teams face challenges that can lead to denials or underpayments.
In this blog, we’ll break down what APCs are, how they differ from similar systems like APGs, the challenges providers often face, and how automation and AI-driven tools can help reduce errors, improve compliance, and accelerate the reimbursement process.
What is an APC?
Ambulatory Payment Classification (APC) is a Medicare payment system for hospital outpatient services. APCs group services that require similar resources and have comparable clinical characteristics. Each group is assigned a payment rate based on the average cost of services within that group.
When a hospital submits a claim for outpatient care, Medicare uses APCs to determine reimbursement. Some services are paid individually, while others may be bundled into a single payment, depending on the nature of the visit. APC payments help cover costs such as medical supplies, labor, and facility overhead.
Structure of APCs
APCs are organized into categories based on the type and complexity of services provided:
- Surgical Procedure APCs: Outpatient surgeries and interventions.
- Significant Procedure APCs: Resource-intensive procedures like chemotherapy, CT/MRI scans, and radiation therapy.
- Medical APCs: Evaluation and management services, such as clinic or emergency department visits.
- Ancillary APCs: Diagnostic tests and treatments, such as X-rays and laboratory tests.
- Composite APCs: Bundled payments for groups of related services, such as imaging with and without contrast.
Physical, occupational, and speech therapy services are not paid under APCs but through a separate Medicare payment system.
APC payment rates are adjusted for geographic differences in labor costs. Modifiers may be used to provide additional information about services, which can sometimes affect payment.
To further enhance your understanding of outpatient reimbursement systems, it's important to recognize that APCs are not the only payment methodology used by healthcare providers.
How is APC different from APG: APC vs APG?
Another system that plays a significant role in determining outpatient reimbursement rates is Ambulatory Patient Groups (APGs). It is a payment methodology used to determine the outpatient reimbursement, primarily by Medicare Advantage Plans and Medicaid programs in certain states.
While APGs share similarities with APCs in their goal of grouping similar outpatient services for reimbursement, they are distinct in several ways. Understanding the distinctions between these two systems is crucial for navigating the outpatient reimbursement landscape effectively, especially when dealing with different payer groups such as Medicare Advantage and Medicaid.
Although both APGs and APCs are used to group outpatient reimbursement purposes, the two systems differ in certain key areas:
APGs are similar to APCs but serve different payer systems, including Medicare Advantage Plans and Medicaid programs in certain states. It's essential for healthcare providers to understand the distinctions between these two systems, as both impact outpatient reimbursement, but they operate in slightly different ways.
How APCs Impact Healthcare Providers
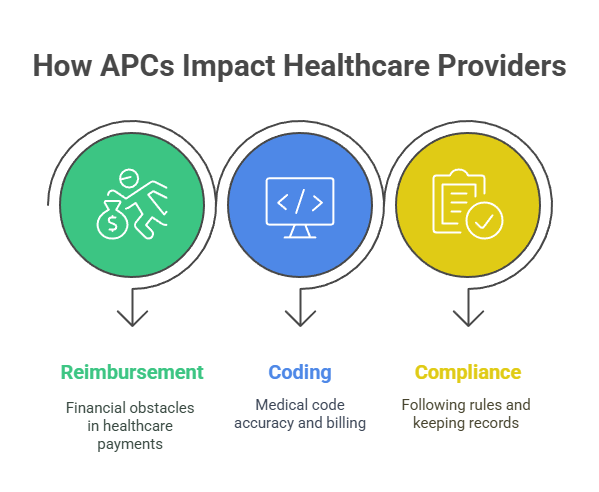
APCs have a direct impact on the financial health of healthcare providers.
Here’s how:
- Reimbursement Challenges: With APCs, hospitals must ensure that each service is properly coded and categorized. If the APC coding is incorrect or incomplete, it can lead to claim denials, delayed payments, or even underpayments. These errors can significantly affect cash flow, making it essential for healthcare providers to ensure accurate coding for all outpatient services.
- Coding Implications: Proper coding is crucial for APCs. Healthcare providers must assign the correct ICD codes (for diagnoses) and CPT codes (for procedures) to each outpatient service. Mistakes in coding can lead to incorrect APC classifications, which in turn affect outpatient reimbursement amounts.
- Compliance and Documentation: Accurate documentation is a key component of the APC process. Missing or inadequate documentation can lead to inaccurate APC assignments. Furthermore, healthcare providers must stay up-to-date with changing regulations and guidelines to ensure ongoing compliance with APC rules and prevent costly errors.
Common APC Challenges and How to Overcome Them
While APCs provide a structured way to categorize outpatient services, they are not without their challenges. Here are some of the most common issues healthcare providers face when working with APCs, along with strategies to overcome them:
- Errors in APC Medical Coding: One of the most common challenges is the assignment of incorrect APC medical codes, which can lead to claim denials or underpayments.
The solution? AI-driven automation significantly reduces human error and improves the accuracy of APC medical coding. By leveraging AI, healthcare providers can reduce the likelihood of coding errors and ensure more accurate outpatient reimbursement.
- Complex Regulations: APC guidelines are frequently updated, which makes it challenging for coders to stay compliant. Providers can address this by implementing AI-powered compliance tools that automatically update their coding systems based on the latest regulations.
With automated updates, AI platforms help providers keep up with changing standards without manual intervention.
- Manual Coding and Documentation: Manual coding is both time-consuming and costly. AI-powered platforms can automate the entire coding process, eliminating the need for human coders to manually assign codes to each service. This automation leads to faster processing, reduced administrative costs, and more efficient use of coding resources.
- Geographic Payment Variations: Since APC reimbursement rates can vary based on geographic location, healthcare providers must stay on top of these adjustments to ensure accurate payments.
AI solutions can help by calculating reimbursement rates based on geographic location and ensuring that each service is billed correctly according to local rates.
How RapidClaims Helps Overcome APC Coding Challenges
Navigating the complexities of APC medical coding can be overwhelming for healthcare providers. From ensuring compliance with changing regulations to handling the manual workload of assigning accurate codes, the challenges are numerous. However, leveraging AI-driven medical coding solutions like RapidClaims can significantly streamline the APC medical coding process.
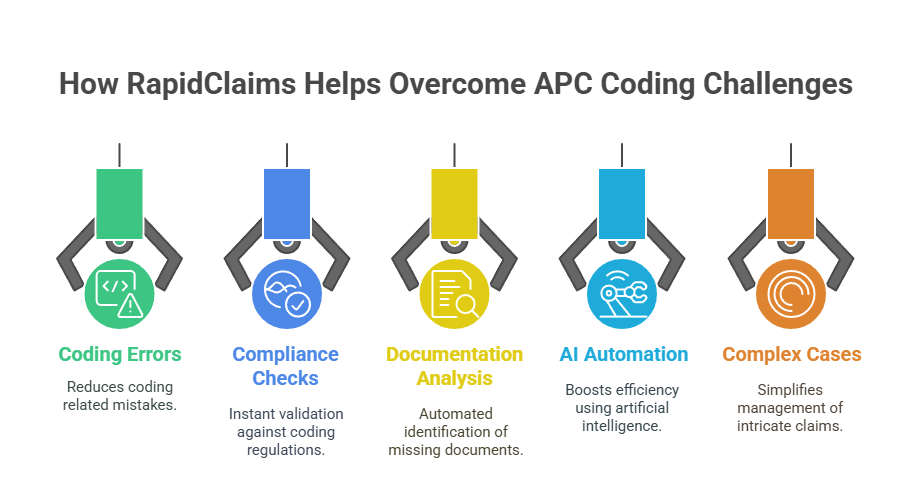
- Minimizing Coding Errors: RapidClaims uses advanced AI algorithms to ensure accurate APC code assignments. By analyzing medical documentation and comparing it with coding guidelines, the platform helps reduce the risk of errors that can lead to claim denials and outpatient reimbursement delays.
- Real-Time Compliance Checks: Staying up-to-date with the latest coding regulations and payment rules can be challenging. RapidClaims integrates real-time compliance checks, ensuring your coding adheres to the most current ICD-10, CPT, and E&M guidelines, reducing the chances of non-compliance and associated penalties.
- Automating Documentation Gap Analysis: One common issue healthcare providers face with APC medical coding is incomplete documentation, leading to underpayments or claim denials. RapidClaims automatically analyzes patient charts to identify missing or inadequate documentation and provides suggestions for improvement, ensuring more accurate and complete claims.
- Improving Efficiency with AI Automation: The manual process of assigning APC medical codes can be time-consuming. With RapidClaims, the automation of coding tasks accelerates the process, allowing healthcare providers to code more charts in less time. This efficiency translates into faster claim submission and quicker reimbursement cycles.
- Handling Complex Cases with Ease: APC coding often requires additional adjustments for complex cases. RapidClaims utilizes AI-powered modifiers to ensure that each service is accurately adjusted for complexity, helping you capture the true value of the care provided and maximizing reimbursement.
With the help of RapidClaims, healthcare providers can not only address common APC coding challenges but also optimize their entire revenue cycle management process. The platform's AI-driven capabilities improve accuracy, reduce manual effort, and ensure compliance, allowing you to focus on what matters most—providing quality care to your patients.
Conclusion:
Ambulatory Payment Classification (APC) plays a pivotal role in ensuring that outpatient services are properly reimbursed. By categorizing services based on the complexity and resources used, APCs help healthcare providers streamline their revenue cycle, improve cash flow, and maintain compliance with ever-changing regulations. However, as we’ve seen, APC coding comes with its own set of challenges, including errors in coding, regulatory complexity, and the need for timely updates.
By understanding the intricacies of APCs, healthcare providers can better navigate these challenges, ensuring that each service is accurately coded and reimbursed. Furthermore, leveraging AI-driven solutions like RapidClaims can greatly enhance the accuracy, speed, and compliance of APC coding, ultimately transforming the reimbursement process for the better.
Ready to take control of your medical coding process and improve your billing accuracy? Schedule your free APC coding audit with RapidClaims today and discover how RapidClaims can help streamline your revenue cycle!
Frequently Asked Questions
1. What is the purpose of the Ambulatory Payment Classification (APC)?
APC is a payment system used by Medicare to determine reimbursement rates for outpatient hospital services. It groups services based on their resource use and the complexity of care, helping establish payment rates for similar outpatient procedures.
2. How are APC payment rates determined?
APC payment rates are determined by the average cost of services within a specific APC group. Factors such as the resources used during treatment, the type of service provided, and geographic location all influence the payment rates.
3. What are the key differences between APC and DRG (Diagnosis-Related Group)?
APCs are used for outpatient services, while DRGs apply to inpatient services. APCs classify individual services or procedures, while DRGs categorize entire hospital stays, including all services provided during the admission.
4. How do APCs affect hospital reimbursement?
APCs directly influence the reimbursement a hospital or healthcare provider receives for outpatient services. Correctly coding and assigning APCs ensures that providers are reimbursed accurately, preventing underpayments or delayed payments.
5. What challenges do healthcare providers face with APC coding?
Challenges include coding errors, regulatory changes, incomplete documentation, and ensuring compliance with the latest guidelines. Incorrect APC coding can lead to claim denials, delayed payments, and compliance issues.
6. Can APCs be adjusted based on the complexity of a patient’s case?
Yes, APCs can be adjusted through the use of modifiers, which account for factors such as higher complexity, additional services, or special circumstances. These adjustments help ensure that payment rates reflect the level of care provided.
%201.png)