Top 10 Revenue Cycle Management Companies in the USA (2026)

The U.S. revenue cycle management market was valued at USD 172.24 billion in 2024. It's projected to grow at a rate of 10.1% annually through 2030. This rapid growth highlights the increasing need for RCM solutions in healthcare organizations.
For revenue cycle managers and compliance officers, managing the revenue cycle effectively has never been more challenging. From coding errors to denied claims, these hurdles can drain resources and impact cash flow. If you’re a healthcare professional, you’re likely familiar with the complexities of balancing patient care and financial stability.
In this blog, we’ll explore the top RCM companies in the U.S., the key factors to consider when choosing an RCM partner, and how these providers can help you overcome common challenges in revenue cycle management.
TL;DR
- RCM Growth: The U.S. RCM market is expanding, with healthcare providers seeking better solutions.
- Top Providers: RapidClaims, CureMD, and others lead with AI tools and cost savings.
- Key Features: Leading companies focus on AI, automation, and data-driven insights to improve accuracy.
- Choosing Partners: Look for providers with scalability, support, results, and industry expertise.
- Measurable Impact: The best RCM companies deliver quick results, reduce denials, and improve overall revenue cycle performance.
Table of Contents:
Top 11 Revenue Cycle Management Companies in 2025
What Do the Best RCM Companies Have in Common?
What to Consider When Choosing Between the Best RCM Companies
Conclusion
FAQs
10 Leading Revenue‑Cycle Management Providers for 2026
The field of revenue cycle management (RCM) is crowded, and selecting the right partner can feel daunting when your team is already managing coding, claims, and collections. You’re looking for a provider that aligns with your size, specialty, and strategic goals.
Below is a strong comparison of top RCM companies in the U.S., giving you a foundation to see where each one might fit your organization.
Comparison Table of Top 10 RCM Companies:
With a clear comparison in mind, let's explore the key features and services provided by the top 10 RCM companies in more detail.
Overview of the Top 10 RCM Companies
Each of the top 10 companies listed in the table offers a range of RCM solutions, from full-service options that handle every stage of the revenue cycle to more specialized tools targeting specific issues like denial management or coding accuracy, or support for medical coders.
Let’s explore each company in greater detail, providing a deeper look at their services, strengths, and ideal client types.
1. RapidClaims
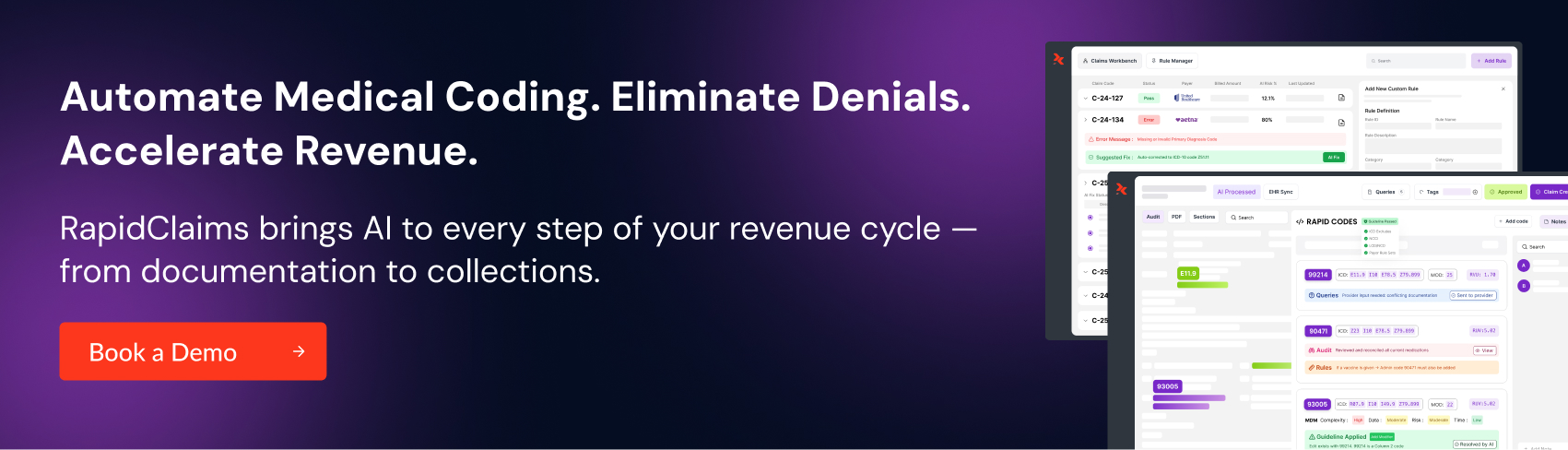
RapidClaims is an enterprise-grade SaaS platform that offers a comprehensive suite of AI-powered solutions for medical coding, denial prevention, and financial performance optimization. The platform is built to help both small practices and large hospitals improve operational efficiency and reduce costs.
- Key Strengths:
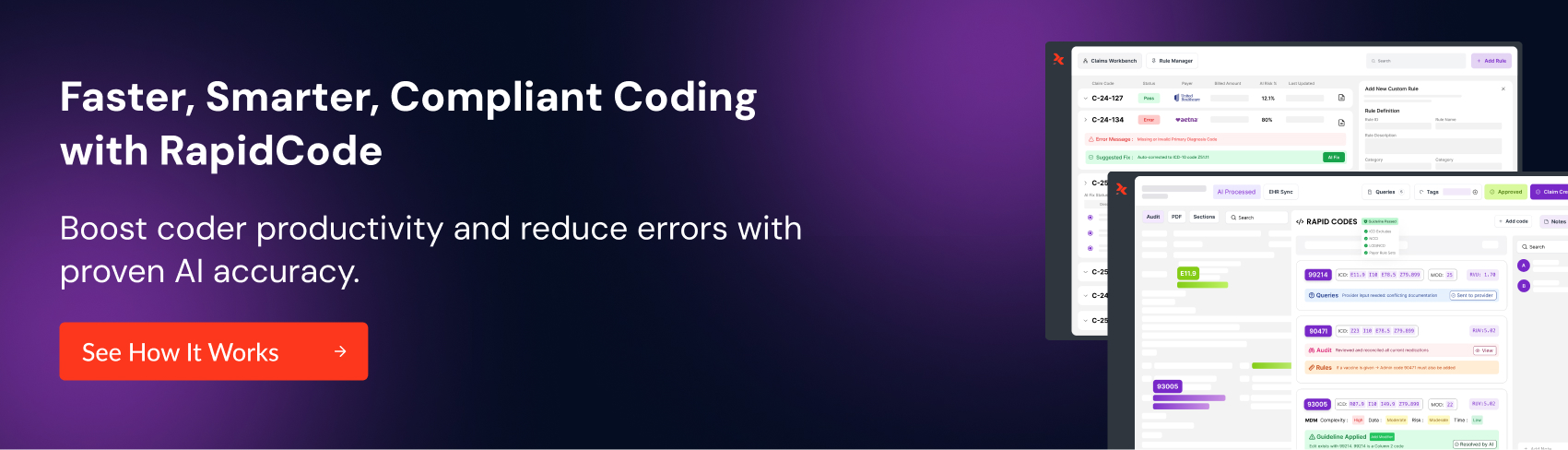
- AI-Driven Technology: RapidClaims automates coding through AI, working alongside tools like RapidCode to improve accuracy and speed in medical coding.
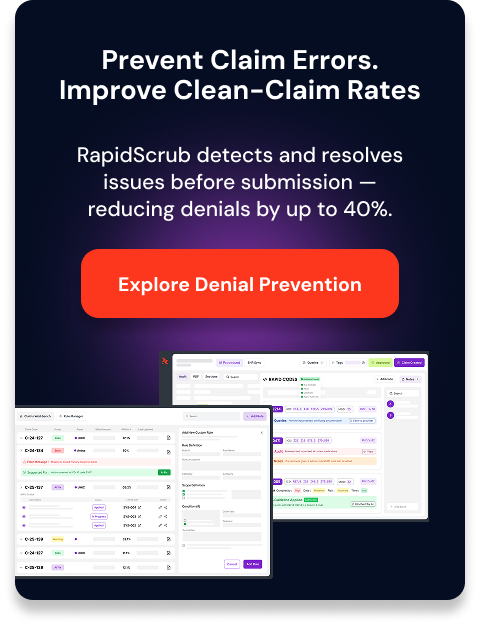
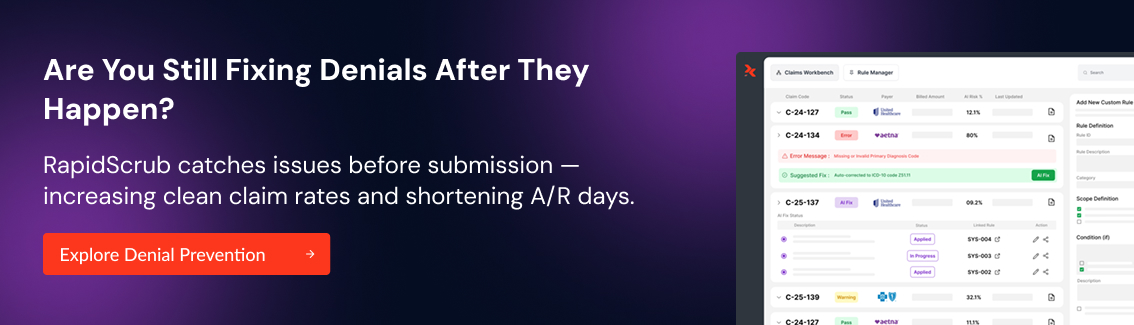
- Fast Results: With tools like RapidScrub and the RapidRules Engine, RapidClaims adapts to revenue cycles quickly, ensuring compliance with payer rules and improving reimbursement rates.
- Cost Savings: Using RapidCDI for better documentation, it lowers the cost to collect by 70%, achieving a return on investment in under a month and boosting productivity by 170%.
- Human + AI Collaboration: By combining AI with human oversight, RapidClaims supports your team, saving more than 2 hours a day by handling routine tasks.
- Best For: Healthcare organizations of all sizes, from small practices to large hospitals, looking for AI-driven solutions that rapidly deliver results and reduce operational overhead.
2. CureMD
CureMD offers an end-to-end RCM service that includes coding, billing, denial management, and reporting. Their platform integrates seamlessly with over 35 billing platforms for easy onboarding and implementation.
- Key Strengths:
- First-Pass Claim Rate: CureMD claims a good first-pass claim rate, minimizing claim denials and speeding up payment cycles.
- Cost Savings: CureMD’s tools help reduce operational costs by up to 60% through simplified workflows and better accuracy.
- Fast Denial Resubmission: With an efficient process in place, CureMD resolves denials within 3 days, ensuring faster reimbursement.
- Best For: Small to medium-sized practices and multi-specialty groups that need a reliable, cost-effective RCM solution.
3. eClinicalWorks
eClinicalWorks provides RCM, EHR, and practice management solutions, with a strong emphasis on insurance verification, claims accuracy, and A/R performance management.
- Key Strengths:
- Scalability: eClinicalWorks’ platform supports growing multi-specialty practices and adapts to increasing billing needs.
- Pre-Authorization and Eligibility Verification: Their integrated tools reduce denials by ensuring that claims are verified before submission.
- A/R Analytics: Offers deep insights into A/R performance, helping practices monitor revenue trends and improve collections.
- Best For: Multi-specialty practices that require a flexible, scalable RCM solution with advanced claims accuracy and A/R tracking capabilities.
4. athenahealth
athenahealth provides cloud-based RCM, predictive analytics, and EHR integration to improve financial performance and reduce claim denials.
- Key Strengths:
- Predictive Analytics: Their AI-driven platform proactively identifies potential claim issues, minimizing errors and denials.
- Seamless Integration: athenahealth’s cloud-based system integrates effortlessly with EHR systems, making it ideal for larger health systems.
- Data-Driven Decision-Making: Provides actionable insights that help practices make better financial decisions and improve operational efficiency.
- Best For: Large healthcare systems or multi-location practices seeking predictive insights, data-driven decision-making, and seamless integration across platforms.
5. R1 RCM
R1 RCM offers full-service RCM solutions, including coding, billing, collections, and financial reporting. Their platform is designed for high-volume claims processing and advanced analytics.
- Key Strengths:
- High-Volume Claims Management: Specialized in handling complex claims at scale, ensuring accuracy and fast reimbursements.
- Advanced Financial Analytics: Provides detailed insights into financial performance, helping healthcare organizations optimize revenue.
- End-to-End Services: R1 RCM’s comprehensive services cover everything from patient access to final payment, ensuring seamless financial operations.
- Best For: Large healthcare systems and hospitals that need an integrated, high-volume solution to manage complex claims and improve financial performance.
6. Greenway Health
Greenway Health provides RCM services, including coding, billing, claims management, and compliance. Their platform also integrates with EHR systems for a comprehensive healthcare solution.
- Key Strengths:
- Compliance Focus: Greenway Health’s platform is tailored to ensure compliance with industry regulations and payer requirements.
- Custom Reporting: Offers tailored reporting tools that help practices track and improve their revenue cycle performance.
- End-to-End Billing and Collections: Provides full-service billing and collections management, reducing delays and errors.
- Best For: Specialty clinics that require robust compliance features, as well as custom reporting and end-to-end billing services.
7. AdvancedMD
AdvancedMD provides RCM, EHR, and practice management solutions with an emphasis on simplifying billing and improving patient engagement.
- Key Strengths:
- Affordable Pricing: AdvancedMD offers subscription-based pricing, making it an affordable option for small practices.
- Patient Engagement: Includes tools like appointment reminders and payment notifications to help improve patient satisfaction and reduce no-shows.
- Automated Payment Posting: Speeds up collections and reduces manual data entry errors with automated workflows.
- Best For: Small to mid-sized practices looking for an affordable, easy-to-use RCM solution with added patient engagement features.
8. Kareo
Kareo offers RCM, EHR, and patient statement solutions designed to simplify billing and payment processes for smaller healthcare providers.
- Key Strengths:
- Simple Interface: Known for its user-friendly interface, Kareo is perfect for solo practitioners or small clinics.
- Low-Cost Solutions: Offers a cost-effective RCM platform that focuses on the essential features—payment processing, patient statements, and collections.
- Quick Set-Up: Fast implementation allows small practices to start using the platform with minimal downtime.
- Best For: Solo practitioners and small clinics that need a straightforward, low-cost RCM solution.
9. Optum360
Optum360 provides full-service RCM solutions with a focus on denial prevention, financial reporting, and analytics. They also offer payer services to help optimize claims submissions.
- Key Strengths:
- Denial Prevention: Strong tools that help prevent denials and ensure smoother claims processing.
- Data-Driven Financial Reporting: Optum360 offers in-depth analytics that help healthcare organizations make informed financial decisions.
- Scalability: Their solutions are highly scalable, making them suitable for both small practices and large health systems.
- Best For: Large healthcare systems that need robust financial analytics and denial prevention tools to improve revenue cycle performance.
10. Conifer Health
Conifer Health offers RCM services, including patient billing, coding, and denial management, with a strong focus on patient satisfaction and financial transparency.
- Key Strengths:
- Expertise in Hospital Billing: Conifer Health specializes in complex hospital billing, making it a strong choice for large health systems and hospitals.
- Patient-Friendly Billing: Their patient billing tools help improve patient satisfaction by providing transparent and understandable billing statements.
- Detailed Financial Reporting: Conifer Health’s platform includes comprehensive financial reporting tools to help organizations improve cash flow and reduce claim denials.
- Best For: Large hospitals and health systems that require specialized billing services and comprehensive financial reporting.
With the top companies identified, let’s now explore the key features that define the best RCM providers.
What Do the Best RCM Companies Have in Common?
Top revenue cycle management companies share several key traits that contribute to their success. These companies focus on delivering results while minimizing operational complexity.

Here are the common characteristics that set the best RCM providers apart:
- Advanced Technology: Leading RCM companies use AI and automation to enhance billing accuracy, prevent denials, and improve operational efficiency.
- Scalability: These companies offer flexible solutions that grow with healthcare organizations, from small practices to large hospital systems.
- Compliance and Security: Top providers ensure compliance with healthcare regulations and safeguard sensitive patient data, minimizing the risk of audits and penalties.
- Data-Driven Insights: The best RCM companies provide in-depth analytics to help healthcare providers make informed decisions and optimize financial outcomes.
- Customer Support: Leading RCM firms offer responsive customer service and ongoing support to ensure clients can address challenges promptly.
- Customizable Solutions: These providers tailor their services to meet the unique needs of each practice or healthcare system, ensuring an optimal fit for various specialties.
Knowing what makes these companies stand out, it’s time to focus on how to choose the right one for your needs.
What to Consider When Choosing Between the Best RCM Companies
When choosing an RCM partner, it’s essential to evaluate several factors that align with your organization’s needs. Key considerations should focus on technology, support, scalability, and overall cost-effectiveness.
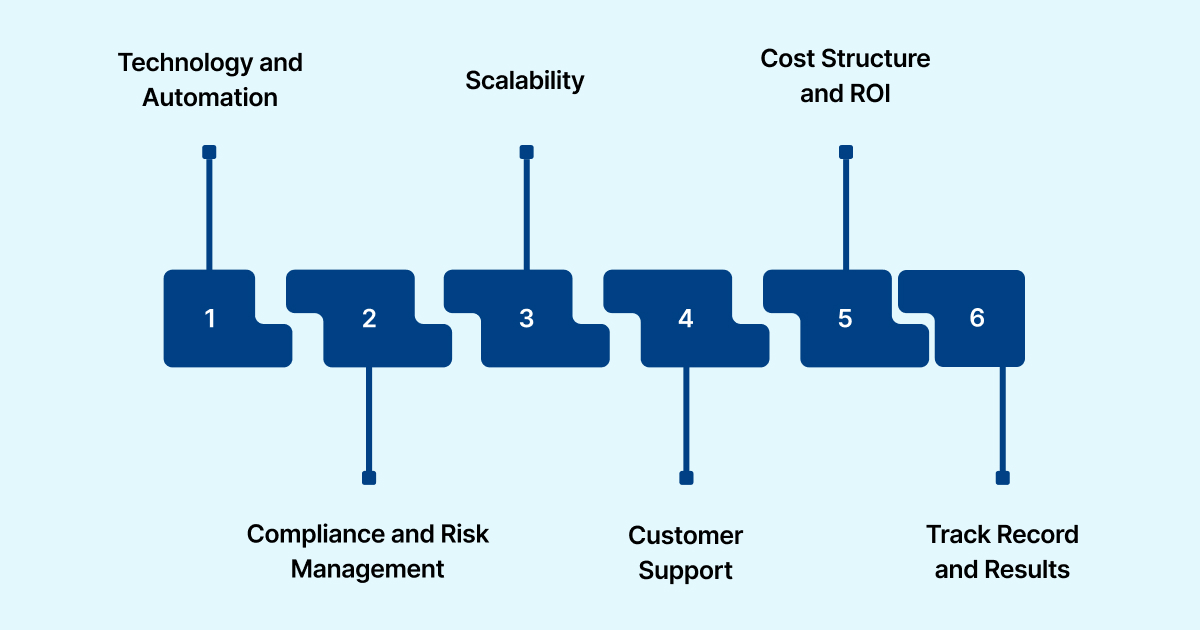
Here are the key factors to keep in mind:
- Technology and Automation: Look for companies that use advanced technology, such as AI and machine learning, to enhance coding accuracy and reduce claim denials.
- Compliance and Risk Management: Ensure the provider complies with healthcare regulations, such as HIPAA, and offers robust data protection measures.
- Scalability: Choose a provider that can scale its services as your practice or healthcare system grows, from small clinics to large hospitals.
- Customer Support: A responsive support team is crucial for addressing issues quickly and ensuring smooth day-to-day operations.
- Cost Structure and ROI: Compare the pricing models and assess whether the service provides measurable improvements in productivity and revenue capture.
- Track Record and Results: Look for companies that provide measurable results, such as reduced AR days, higher clean claim rates, and improved reimbursement rates.
Considering these factors, RapidClaims excels with its AI-driven tools that dramatically reduce denials, deliver measurable results within 30 days, and offer seamless scalability to fit various healthcare needs.
Conclusion
Choosing the right RCM company is crucial for optimizing your healthcare organization’s financial performance. The best providers offer technology, support, scalability, and measurable results.
RapidClaims stands out with AI-driven solutions that reduce denials and improve coding accuracy. The platform delivers quick results, helping healthcare organizations see an impact within 30 days.
If you're ready to boost your revenue cycle management, request a demo to see how it can improve your financial outcomes today.
FAQs
1. What are the three key components of Revenue Cycle Management?
The three key components of RCM are coding, billing, and collections. These processes ensure accurate patient records, timely claim submissions, and proper payment collection.
2. What does the "4 P's" refer to in the revenue cycle?
The "4 P's" in the revenue cycle are Patient, Provider, Payer, and Payment. These elements represent the stakeholders and steps involved in the financial transaction process.
3. How does RCM impact a healthcare provider's financial health?
RCM helps providers improve cash flow by reducing claim denials, speeding up payment processing, and optimizing billing and collections to ensure timely reimbursements.
4. What are the fundamental principles behind effective revenue management?
The core principles include accuracy in coding, timely claims submission, follow-up on unpaid claims, and maintaining compliance with regulations.
5. How do RCM companies help reduce claim denials?
RCM companies reduce denials by ensuring correct coding, verifying patient insurance information, and proactively identifying potential issues before submitting claims.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






