.webp)
Pediatric Billing and Coding Guide for Accurate Claims

A JAMA Network Open 2024 study of 450,146 pediatric patients found that 9% were disenrolled from Medicaid to uninsured status through March 31, 2024. This highlights a critical challenge for pediatric practices: ensuring accurate billing and coding while maintaining insurance coverage.
For billing teams, this emphasizes the need to combine precise pediatric billing and coding with real-time eligibility verification. By doing so, practices can reduce claim denials, minimize revenue loss, and maintain seamless care continuity for pediatric patients.
In this blog, you’ll learn the essentials of pediatric billing and coding, and identify claim error sources to optimize reimbursements while ensuring care continuity.
TL;DR (Key Takeaways)
- Accurate coding using the correct CPT, ICD-10, and HCPCS codes ensures proper reimbursement and reduces claim denials.
- Understanding developmental stages from neonate to adolescence is essential for selecting appropriate codes and procedures.
- Precise documentation of well-child visits, immunizations, and counseling supports claims and regulatory compliance.
- Utilizing technology and AI platforms, such as RapidClaims, streamlines coding, minimizes errors, and improves revenue cycle efficiency.
- Continuous staff training, internal audits, and expert support help maintain compliance with evolving coding guidelines and reduce administrative risks.
Table of Contents:
- What Is Pediatric Billing and Coding?
- Key Pediatric Billing and Procedure Codes for Accurate Claims
- Essential Pediatric Vaccine Codes for Accurate Billing
- Essential Documentation Practices for Pediatric Billing
- Importance of Accurate Coding for Reimbursement
- Overcoming Common Pediatric Billing Challenges
- Key Strategies for Effective Pediatric Billing and Coding
- Conclusion
- Frequently Asked Questions (FAQs)
What Is Pediatric Billing and Coding?
Pediatric billing and coding involves applying the correct CPT, ICD-10, and HCPCS codes for patients from newborns to adolescents to ensure accurate communication with payers and proper reimbursement. It requires a strong understanding of age-specific codes, procedural nuances, and documentation standards.
Pediatrics covers the physical, mental, and social health of children from birth to young adulthood, across specialties such as neonatology, pediatric emergency medicine, critical care, cardiology, rheumatology, pulmonology, and developmental-behavioral pediatrics. Understanding the unique needs of each age group is essential for coding professionals to submit accurate claims and ensure timely reimbursement.
Below is a breakdown of age groups commonly used in pediatric billing, serving as a reference for selecting appropriate codes for each patient population:
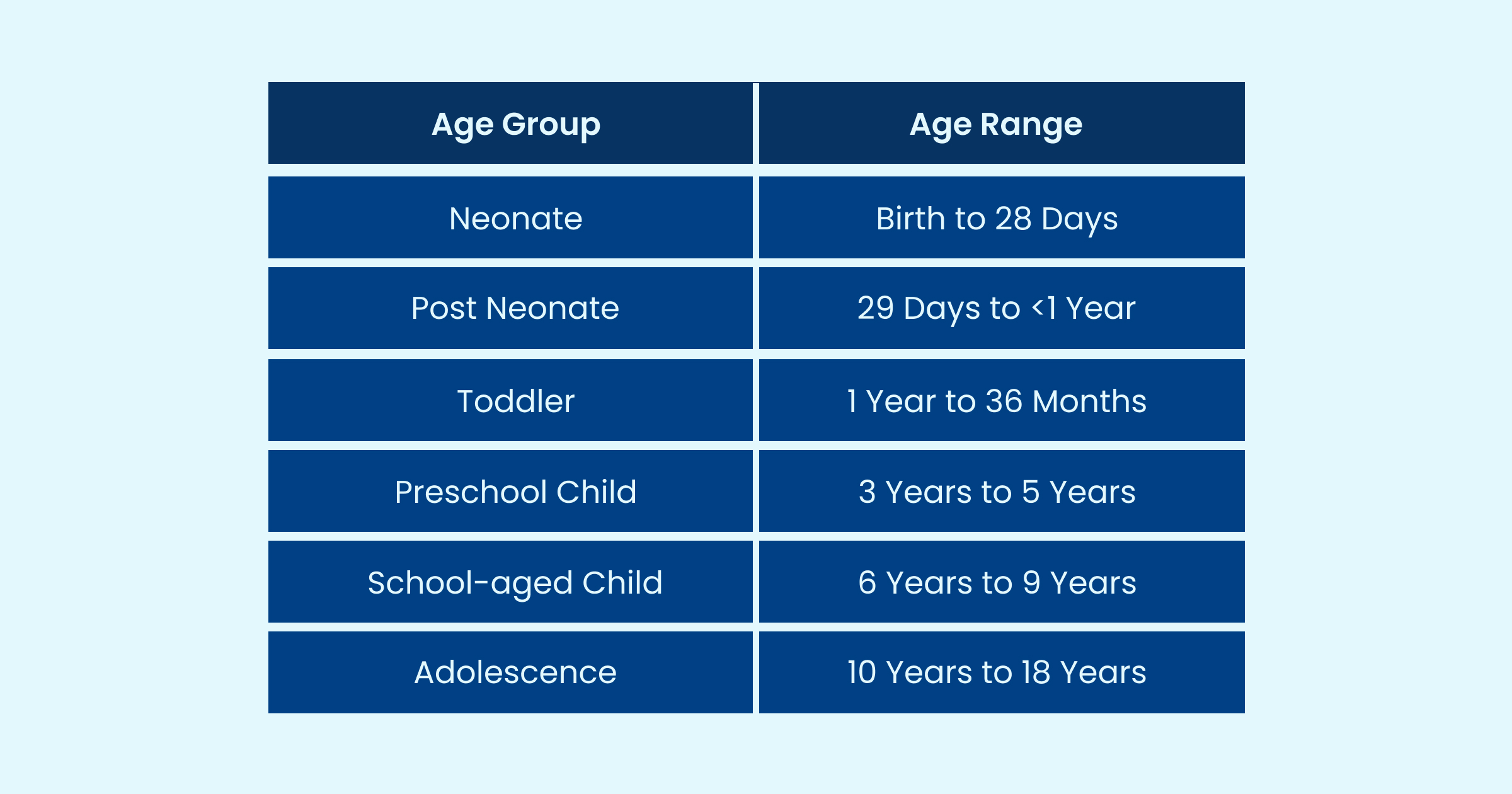
With a clear understanding of age groups and specialties, the next step is to review the common pediatric billing and procedure codes used for accurate claims submission.
Key Pediatric Billing and Procedure Codes for Accurate Claims
Accurate pediatric billing relies on selecting the correct codes for evaluation, preventive care, and procedures. E&M codes are essential for documenting patient encounters, with the choice of code reflecting the visit’s complexity, duration, and the patient’s medical needs. Preventive medicine codes encompass routine well-child visits, growth assessments, and immunizations, all of which are crucial for maintaining a child's overall health.
In addition, procedure codes cover pediatric-specific interventions, surgical procedures, and treatments unique to this population. Understanding these codes ensures claims are correctly submitted, reduces denials, and supports compliance with payer requirements.
Key Pediatric Codes:
- 54150: Circumcision performed using a clamp or other device.
- 54160: Surgical circumcision procedures.
- 36510: Insertion of a central venous catheter.
- 90460: Vaccine administration with counseling for the patient or caregiver.
- 90461: Vaccine administration without counseling.
- 99202–99205: Office or outpatient visits for new patients, coded according to complexity and services provided.
- 99211–99215: Office or outpatient visits for established patients, selected based on visit level and clinical requirements.
- 99381–99384: Preventive visits for new patients, covering growth, development, and initial health assessments.
- 99391–99394: Preventive visits for established patients, including routine check-ups, immunizations, and counseling.
Example: A 4-year-old established patient comes in for a routine well-child visit with immunizations. The coder selects 99392 for the preventive visit and 90461 for vaccine administration without counseling. Proper coding ensures the claim is approved without denials.
The codes are organized by patient age and whether the patient is new or established to the practice. This framework aligns with the American Academy of Pediatrics' Pediatric Billing and Coding Guidelines, enabling practices to reduce denials and maintain compliance.
Let’s review the essential pediatric vaccine codes that ensure accurate billing, proper documentation, and timely reimbursement for preventive care services.
Essential Pediatric Vaccine Codes for Accurate Billing
Vaccination is a critical component of pediatric care, and accurate coding ensures proper documentation, timely reimbursement, and compliance with preventive care guidelines. Using the correct vaccine codes also reduces claim denials and supports the overall revenue cycle.
Key Pediatric Vaccine Codes:
- 90686: Influenza virus vaccine, quadrivalent (IIV4), split virus, preservative-free, 0.5 mL, intramuscular use.
- 90688: Influenza virus vaccine, quadrivalent (IIV4), split virus, 0.5 mL, intramuscular use.
- 91318: SARS-CoV-2 (COVID-19) mRNA-LNP vaccine, 3 mcg/0.3 mL, tris-sucrose formulation, intramuscular use.
- 90633: Hepatitis A (HepA) vaccine, pediatric/adolescent, 2-dose schedule, intramuscular use.
- 90744: Hepatitis B vaccine, pediatric/adolescent, 3-dose schedule, intramuscular use.
- 90707: Measles, mumps, and rubella (MMR) vaccine, live, subcutaneous use.
Example: A 6-month-old receives the Hepatitis B and DTaP vaccines in a single visit. The coder should report:
- 90744 for the Hepatitis B vaccine (pediatric/adolescent dosage, 3-dose schedule, for IM use)
- 90700 for the DTaP vaccine (Diphtheria, tetanus toxoids, and acellular pertussis vaccine, when administered to children under 7 years, for IM use)
- 90461 for the administration of each additional vaccine component beyond the first, without counseling.
This coding approach ensures that both vaccines are reimbursed correctly and complies with the guidelines of the American Academy of Pediatrics.
For detailed information and updates on pediatric vaccine coding, you can refer to the AAP Immunization Coding Table, which lists all the correct codes for accurate claim submission. Additionally, the Current CDC Vaccine Price List provides updated vaccine costs, helping coders verify charges for precise billing.
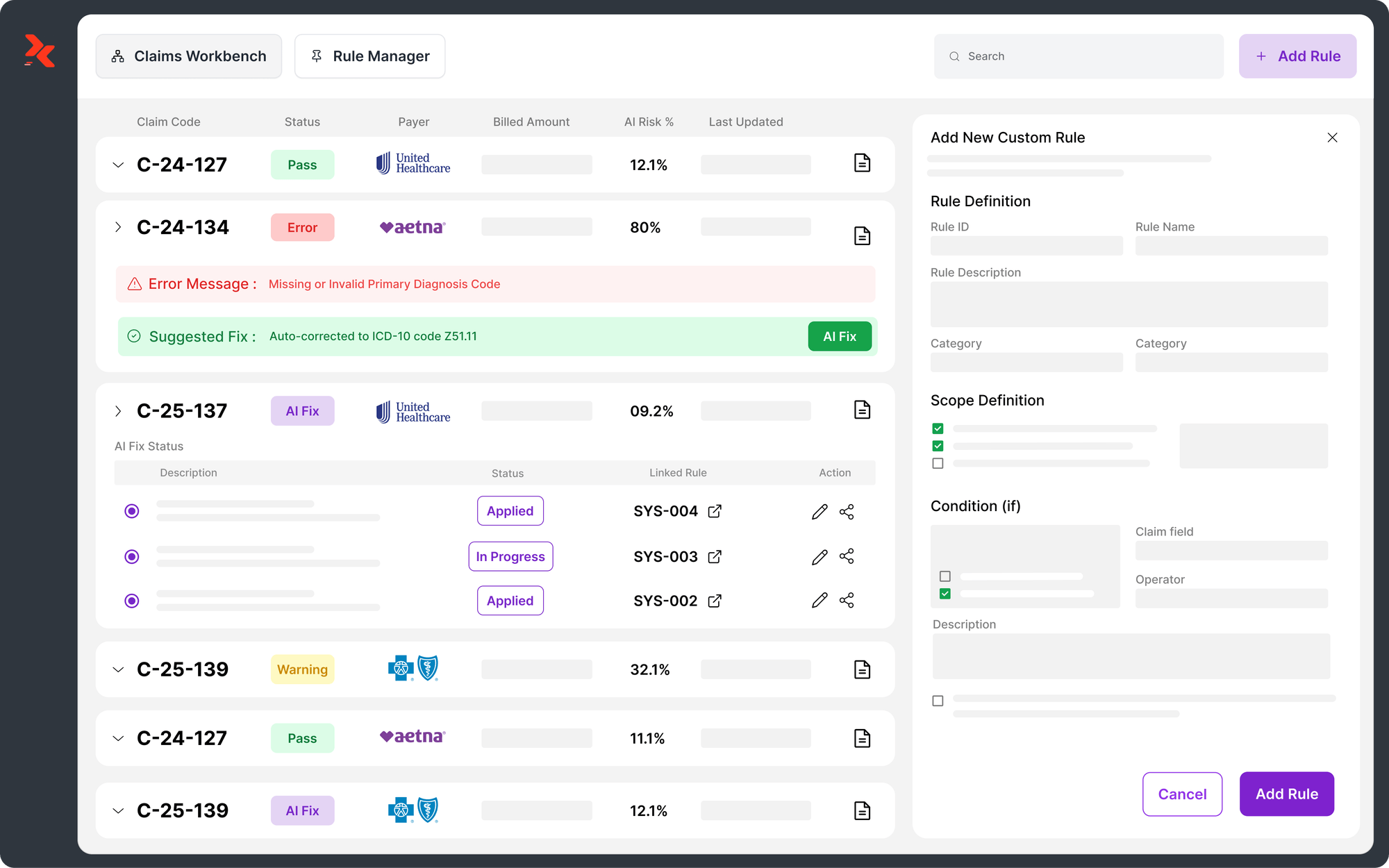
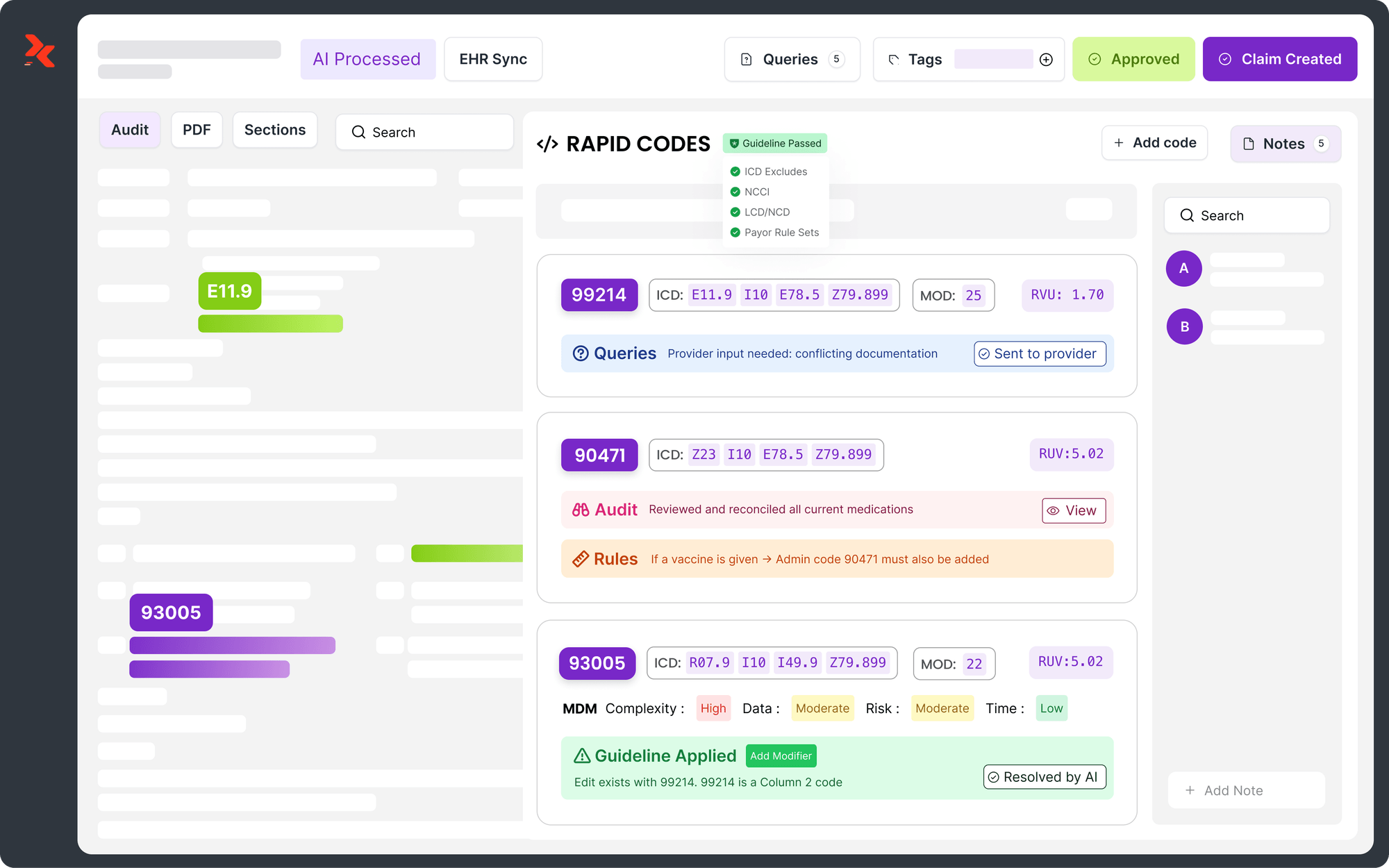
Managing multiple vaccine codes and staying up-to-date with frequent guideline changes can be time-consuming. AI-powered platforms like RapidClaims delivers end-to-end revenue-cycle automation, helping pediatric practices achieve a 98 % clean-claim rate and 30-day time-to-value. With automated coding, denial prevention, and seamless EHR integration, practices can reduce administrative costs, minimize claim denials, and focus more on patient care.
Key Documentation Practices for Accurate Pediatric Billing
Accurate and thorough documentation is crucial for pediatric billing. It supports claim approval, minimizes denials, and ensures compliance with payer and regulatory requirements. The following key elements should be consistently recorded:
- Patient history and developmental assessment: Document past medical history, family health background, social determinants, and age-appropriate physical, cognitive, and behavioral milestones.
- Physical exam and procedure notes: Record all relevant observations, measurements, and detailed notes for procedures such as circumcision or catheter insertion.
- Vaccinations and counseling: Include vaccine dates, dosages, and any counseling provided to caregivers.
- Consent, follow-up, and care coordination: Ensure parental/guardian consent, referrals, specialist communication, and follow-up plans are clearly documented.
- Medication and allergy reconciliation: Maintain updated medication lists and allergy information for each visit.
- Time-based and telehealth documentation: Note the duration of counseling, teaching, or complex decision-making, and document the telehealth platform, consent, and visit duration when applicable.
Thorough and precise documentation is crucial for effective pediatric billing; however, managing multiple codes, procedures, and regulatory requirements can be a challenging task. RapidClaims, an AI-powered platform, automates coding, integrates with EHRs, and ensures compliance. With a 98 % clean-claim rate, 40 % fewer denials via RapidScrub, and boosted productivity through RapidCode, practices can reduce errors, accelerate reimbursements, and focus on patient care.
Importance of Accurate Coding for Reimbursement
Accurate coding is the key element of pediatric billing, directly impacting reimbursement, compliance, and revenue cycle efficiency. Precise coding ensures that services provided are correctly represented to payers and that claims are processed without delays or denials.
Key Reasons Accurate Coding Matters:
- Proper Reimbursement: Correct CPT, ICD-10, and HCPCS codes ensure providers are paid appropriately for services rendered.
- Reduced Claim Denials: Accurate coding minimizes errors that lead to claim rejections or requests for additional documentation, ultimately reducing the likelihood of denials.
- Compliance with Regulations: Coding in line with payer and regulatory requirements prevents audits, penalties, and legal issues.
- Care Continuity: Accurate documentation supports clinical decision-making and ensures patient records reflect true care delivered.
- Efficient Revenue Cycle: Reduces administrative burden and accelerates cash flow by preventing resubmissions and appeals.
Despite best efforts, pediatric billing presents recurring challenges; let’s identify and address them.
Overcoming Common Pediatric Billing Challenges

Pediatric billing involves several unique complexities that can affect reimbursement, compliance, and practice efficiency. Common challenges include:
1. Inconsistent Documentation
Variations in how providers record patient history, physical exams, procedures, and counseling can lead to coding errors, claim denials, and audit risks. Standardized templates and staff training can minimize these inconsistencies.
2. Complex Payer Requirements
Medicaid, CHIP, and state immunization programs often have specific eligibility, coverage, and documentation rules. Misunderstanding these regulations can result in delayed or denied claims, making ongoing staff education and eligibility verification essential.
3. Frequent Code Updates
CPT, ICD-10, and HCPCS codes are updated annually. The 2025 updates include changes for telehealth services, vaccines, and remote patient monitoring. Staying current is crucial to ensure accurate coding and avoid underpayment or denials.
4. Coordination of Benefits
Pediatric patients often have multiple insurance plans. Incorrect coordination of primary and secondary payers can delay claim processing and reimbursements. Implementing automated eligibility checks and verification workflows can reduce delays.
By proactively addressing these challenges, pediatric practices can improve claim accuracy, accelerate reimbursement, and maintain compliance with evolving healthcare regulations.
With those challenges in mind, here are key strategies to enhance your pediatric billing and coding.
Key Strategies for Effective Pediatric Billing and Coding

Implementing well-defined strategies is crucial for pediatric practices to improve coding accuracy, reduce claim denials, and ensure timely reimbursements. These approaches streamline workflows while ensuring compliance with evolving healthcare regulations.
- Stay Current with Coding Updates
Track annual CPT, ICD-10, and HCPCS changes, including 2025 updates for telehealth, vaccines, remote patient monitoring (RTM), and E/M simplifications. Staying up-to-date prevents coding errors and ensures proper reimbursement.
- Ongoing Staff Training
Invest in pediatric coding certifications and use resources such as AAP preventive care guidelines and real-world case vignettes. Continuous education strengthens coding accuracy and compliance.
- Use Cheat Sheets & Documentation Tools
Quick-reference tools for well visits, sick visits, vaccines, telehealth, and newborn care help streamline coding and minimize errors.
- Utilize Technology
Pediatric-specific EHRs with auto-coding, real-time eligibility verification, and proactive code updates improve efficiency and reduce administrative burden.
- Conduct Internal Audits
Regular chart reviews identify errors early, allowing corrective actions and ongoing staff development to maintain coding quality.
- Partner with Pediatric Billing Experts
Outsourcing to specialized pediatric billing teams can help navigate complex codes, enhance documentation, and optimize reimbursement for preventive and vaccine services.
Pro Tip: Implementing these strategies together, including continuous education, technology use, audits, and expert support, ensures accurate pediatric coding. It also helps reduce claim denials and maximizes timely reimbursements.
Conclusion
Accurate pediatric billing and coding are essential for efficient revenue cycles and audit readiness. With 2025 CPT updates, simplified E/M guidelines, and changes to preventive care coding, healthcare teams must stay informed, train regularly, and adopt reliable tools.
To streamline these processes and minimize errors, healthcare teams can utilize AI-powered solutions like RapidClaims, which automate coding, prevent denials, and provide real-time reporting. These features speed up claims, enhance reimbursements, and ensure audit readiness, letting providers focus on quality pediatric care.
Want to Enhance Your Pediatric Coding Process? See how RapidClaims helps practices reduce errors, speed up claims, and stay audit-ready. Request a Free Demo to explore smart, AI-powered solutions for accurate pediatric medical coding.
Frequently Asked Questions (FAQs)
1. How can I ensure accurate coding for pediatric preventive care visits?
A. Use the correct E/M codes based on patient age and visit complexity. Codes 99381–99385 apply to new patients, while codes 99391–99394 apply to established patients. Document history, examination, and counseling to support the code.
2. How do I handle coding when a child receives multiple vaccines in a single visit?
A. Report each vaccine using its specific CPT or HCPCS code and include the appropriate administration code (90460 if counseling is provided, 90461 if not). Clearly document the vaccine type, dosage, route, and any counseling or guidance given to caregivers to ensure accurate claims and reimbursement.
3. How do I code a comprehensive health assessment within 30 days of a child's placement?
A. Bill as a well-child exam using 99381–99384 for new patients and 99391–99394 for established patients. Ensure documentation reflects the full assessment.
4. What is the significance of modifiers in pediatric billing?
A. Modifiers give additional details about a service or procedure. For example, Modifier 25 indicates a separate E/M service on the same day. Correct use prevents denials and ensures proper reimbursement.
5. How do I code for telehealth visits in pediatric care?
A. Use the same CPT/E/M codes as in-person visits, adding the appropriate telehealth modifier (e.g., 95). Document the platform used, patient consent, and the duration of the visit. Ensure all services provided, including counseling or procedures, are clearly recorded to support accurate reimbursement.
Latest Post
What Does Current Procedural Terminology Mean and Why Is It Important in Medical Coding?
How Does AI Reduce Denials and Boost Efficiency in Medical Billing?
DRG Validation in 2026: Why is it Essential for Hospitals?
EMR Conversion Challenges & Best Practices in 2026
CO 11 Denial Code: What It Means and How to Fix It
Related Post
Top Products
%201.png)