Differences between Fee-for-Service and Value-Based Care

For decades, fee-for-service (FFS) has been the standard approach to healthcare reimbursement. Providers are paid separately for each service they perform, whether it is a test, procedure, or consultation. While this model is easy to understand, it often encourages a higher volume of services such as tests and procedures rather than focusing on the quality of care or patient outcomes.
In response to rising costs and fragmented care, value-based care (VBC) has emerged as a more outcome-driven alternative. Instead of rewarding volume, VBC emphasizes clinical effectiveness, patient satisfaction, and cost efficiency.
Understanding the key differences between FFS and VBC is critical for healthcare organizations, providers, and administrators. The payment model in use directly shapes care delivery, revenue cycles, compliance strategies, and long-term sustainability.
This blog breaks down how these models differ in structure, incentives, and outcomes to help you make informed decisions about your healthcare operations.
TL;DR: Fee for Service vs Value Based Care
- Fee for Service (FFS) pays providers per individual service, often prioritizing quantity over care outcomes
- Value Based Care (VBC) rewards providers for quality, efficiency, and long term patient outcomes
- Claims and Coding workflows shift significantly as FFS is volume driven while VBC emphasizes accuracy, compliance, and data driven reporting
- Industry Shift shows CMS and payers pushing for broader adoption of value based models like ACOs and bundled payments
- Understanding these differences is essential for optimizing reimbursement, care delivery, and operational strategy
What Is Fee-for-Service (FFS)?
Fee-for-service is a traditional payment model where healthcare providers are reimbursed for each individual service rendered. Every test, procedure, or visit generates a separate charge, regardless of the outcome or coordination with other care.
Key Characteristics of Fee-for-Service:
- Payment Structure: Providers bill for each unit of care such as exams, lab tests, imaging, surgeries, and follow-ups
- Incentive Model: Revenue increases with the number of services delivered, creating a volume-focused environment
- Care Coordination: Often leads to fragmented care as there is no built-in incentive to collaborate across providers
- Risk Distribution: Financial risk remains with payers since providers are paid regardless of results or efficiency
- Compliance Focus: Documentation is centered around procedure justification and code-level accuracy for billing purposes
This model remains dominant in many healthcare systems but is increasingly scrutinized for its role in driving up costs without consistently improving outcomes.
What Is Value-Based Care?
Value-based care is a healthcare delivery and reimbursement model that rewards providers based on the quality and outcomes of care rather than the volume of services delivered. It emphasizes prevention, care coordination, and long-term patient health.
Key Characteristics of Value-Based Care:
- Payment Structure: Providers are reimbursed based on clinical outcomes, cost-efficiency, and patient experience
- Incentive Model: Encourages proactive, coordinated care that reduces avoidable hospitalizations and improves population health
- Care Coordination: Requires integration among primary care, specialists, and support services to align around patient needs
- Risk Distribution: Shifts some financial responsibility to providers, incentivizing them to control costs and reduce complications
- Compliance Focus: Involves strict adherence to quality metrics, outcome reporting, and accurate risk adjustment documentation
This model aligns better with long-term health goals and payer expectations and is often supported by frameworks like ACOs, bundled payments, and shared savings programs.
Fee-for-Service vs. Value-Based Care: A Side-by-Side Comparison
How Fee-for-Service and Value-Based Care Models Affect Claims and Coding
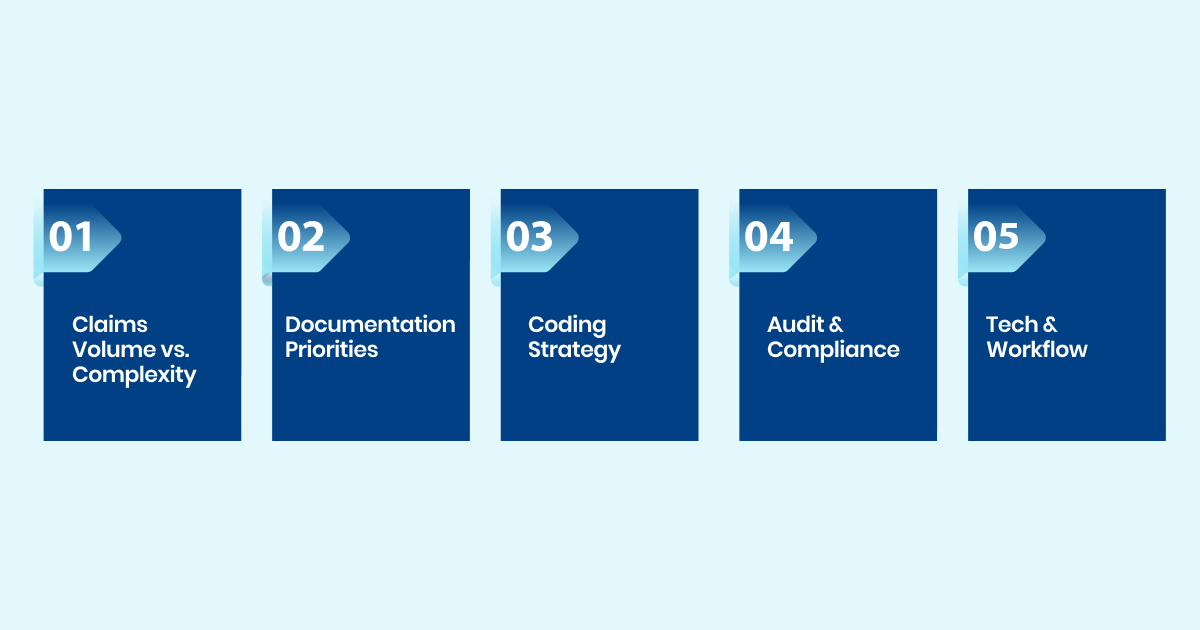
Both Fee-for-Service and Value-Based Care models shape how claims are submitted and how coding workflows are designed; here’s how they differ behind the scenes:
1. Claims Volume vs. Complexity
- FFS models result in higher claim volumes with simpler service-level codes.
- VBC models involve fewer claims but require more nuanced, outcome-aligned coding.
2. Documentation Priorities
- Under FFS, emphasis is on procedure quantity and code accuracy.
- VBC prioritizes clinical justification, care outcomes, and risk stratification.
3. Coding Strategy
- FFS relies on detailed service coding, often disconnected from overall care goals.
- VBC demands coordinated coding that reflects longitudinal care and patient complexity.
4. Audit and Compliance Scope
- FFS audits focus on billing accuracy and fraud prevention.
- VBC audits assess quality reporting, risk adjustment, and adherence to outcome measures.
5. Technology and Workflow Needs
- FFS workflows can function in silos; coding is often post-visit.
- VBC requires integrated systems that support real-time documentation, coding, and quality tracking.
Is the Industry Really Shifting to Value-Based Care?
Evidence shows the shift toward value-based payment is accelerating through government and payer initiatives.
- As of January 2025, 53.4 percent of traditional Medicare beneficiaries are part of an accountable care arrangement. This marks a 4.3 percentage point increase from the previous year and now includes more than 14.8 million individuals.
- In 2024, CMS reported 13.7 million Medicare fee-for-service beneficiaries were aligned with ACOs, reflecting a 3 percent rise compared to 2023.
- According to the Health Care Payment Learning & Action Network, nearly 60 percent of healthcare payments in 2020 included quality or value components, up from 53 percent in 2017.
These trends reflect growing support for outcome-driven care across Medicare and private payers.
How can providers adapt?
- Implement interoperable technology and care coordination platforms that support data sharing across systems
- Refine clinical documentation and coding to accurately reflect outcomes, risk levels, and quality benchmarks
- Build scalable infrastructure that supports ACO participation, bundled payments, and shared savings models
Adopting these strategies now positions providers to thrive in an increasingly value-focused reimbursement landscape.
How RapidClaims Supports Both Models

Whether your organization operates under a traditional fee-for-service structure or is transitioning toward value-based care, RapidClaims provides the flexibility and compliance intelligence to support both.
- For Fee-for-Service Models: RapidClaims automates CPT, HCPCS, and ICD-10 code validation at the point of care to ensure every billable service is accurately captured. This reduces manual rework and improves first-pass claim rates across high-volume procedures.
- For Value-Based Care Models: The platform embeds quality metric tracking, risk adjustment support, and documentation alignment with care outcomes. It helps ensure coding reflects clinical complexity and meets payer-specific quality thresholds.
- Unified Claim Preparation for Mixed Models: RapidClaims supports organizations managing hybrid payment environments by applying payer-specific logic during charge entry. Whether a claim falls under bundled payments or fee-for-service, compliance and audit readiness are maintained consistently.
By adapting to both reimbursement structures, RapidClaims enables healthcare providers and coders to remain agile and accurate while meeting evolving payer requirements.
Final Thoughts
The move from fee for service to value based care represents more than a shift in payment; it redefines how accountability, quality, and coordination are measured in healthcare. Providers are no longer evaluated solely on the number of services delivered but on how well those services translate into real health outcomes.
This shift requires smarter systems that can interpret clinical data in real time, validate codes based on payer-specific rules, and align documentation with both financial and care goals.
RapidClaims fits right into this new reality. It is more than a billing engine; it helps ensure your claims process remains compliant, efficient, and outcome oriented, regardless of the payment model.
The question now is not whether value based care is coming. It is whether your technology can keep pace with it.
Request a Demo and see how RapidClaims makes your revenue cycle ready for what is next.
Frequently Asked Questions
1. What are the key differences between fee for service and value based care?
Ans: Fee for service reimburses providers per service performed, encouraging volume over outcomes. Value based care ties payments to health outcomes, cost efficiency, and patient satisfaction, promoting coordinated, quality care.
2. How does value based care incentivize providers?
Ans: Providers earn more by meeting quality metrics such as reduced hospital readmissions and improved A1C levels. This model encourages preventive care and coordination.
3. What payment models are used in value based care?
Ans: Common models include accountable care organizations (ACOs), bundled payments, shared savings, shared risk contracts, and capitation. All these models align payment with outcomes.
4. What are the advantages of value based care?
Ans: This model improves patient outcomes, enhances care coordination, and reduces costs by emphasizing preventive care over unnecessary services.
5. What challenges arise when transitioning from fee for service to value based care?
Ans: Providers face greater financial risk, need to invest in technology and data systems, and must adapt to outcome based metrics.

Muyied Ulla Baig
Muyied Ulla Baig is a dedicated medical coder with 1 year of experience in E/M Outpatient, HCC, and Dental coding, supporting accurate risk adjustment and claims integrity through detailed and compliant coding processes at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






