Utilizing Data for Value-Based Care Improvement
.jpg)
Healthcare is shifting away from volume-based payment models toward ones that reward better outcomes, fewer complications, and long-term cost efficiency. This shift is known as value-based care (VBC); and it's transforming how providers deliver care, how payers reimburse, and how performance is measured.
But for value-based care to work, one element is absolutely critical: data.
Data now drives not just clinical decisions, but risk adjustment, compliance, reimbursement, and patient engagement. In this blog, we’ll break down what data-driven value-based care really looks like, where organizations struggle most, and how the right tools can turn documentation into measurable results.
For healthcare teams, the implications are significant. Clinical staff, coding specialists, and revenue cycle leaders must all work from the same data foundation. Without clean, actionable insights guiding each step; from documentation to reimbursement; organizations risk falling short of performance targets, missing incentives, or delivering fragmented care.
TL;DR (Key Takeaways)
- Value-based care depends on structured, codified, and interoperable data. Data is no longer passive; it directly influences reimbursement, quality scoring, and care planning.
- Clinical documentation is also a financial function. Each data point contributes to coding accuracy, risk adjustment, and performance metrics.
- The challenge is not data availability, but data usability. Siloed systems, inconsistent inputs, and a lack of real-time validation prevent meaningful action.
- Legacy systems limit the scalability of value-based care. Without AI, automation, and interoperability, meeting payer expectations becomes increasingly difficult.
- Tools like RapidClaims connect clinical input to financial outcomes. AI-powered coding suggestions, built-in compliance checks, and real-time insights streamline both documentation and reimbursement.
Understanding Value-Based Care and the Role of Data in Making It Work
Beyond the shift in payment structure, value-based care introduces new expectations around how care is delivered, tracked, and justified. It encourages proactive treatment plans, coordinated provider efforts, and a focus on long-term patient well-being.
How data supports these expectations:
- Aligns care with measurable outcomes: Data helps monitor quality metrics such as patient satisfaction, medication adherence, and recovery timelines.
- Reveals care gaps in real time: Providers can use clinical data to identify missed screenings, follow-ups, or preventive services.
- Enables personalized care planning: Combining historical and real-time data allows for more tailored interventions, especially for patients with chronic or complex conditions.
- Improves collaboration across teams: Shared access to clinical notes, test results, and prior treatments helps care teams make informed, timely decisions.
- Reduces the risk of errors and omissions: When data is centralized and structured, it lowers the chances of duplicative tests, missed diagnoses, or non-compliant billing.
Core Components of Data-Driven Value-Based Care
Data alone does not improve care or secure reimbursements. The value lies in how well that data is structured, interpreted, and used to support clinical and financial decisions. Below are the essential components that power an effective data-driven approach to value-based care.
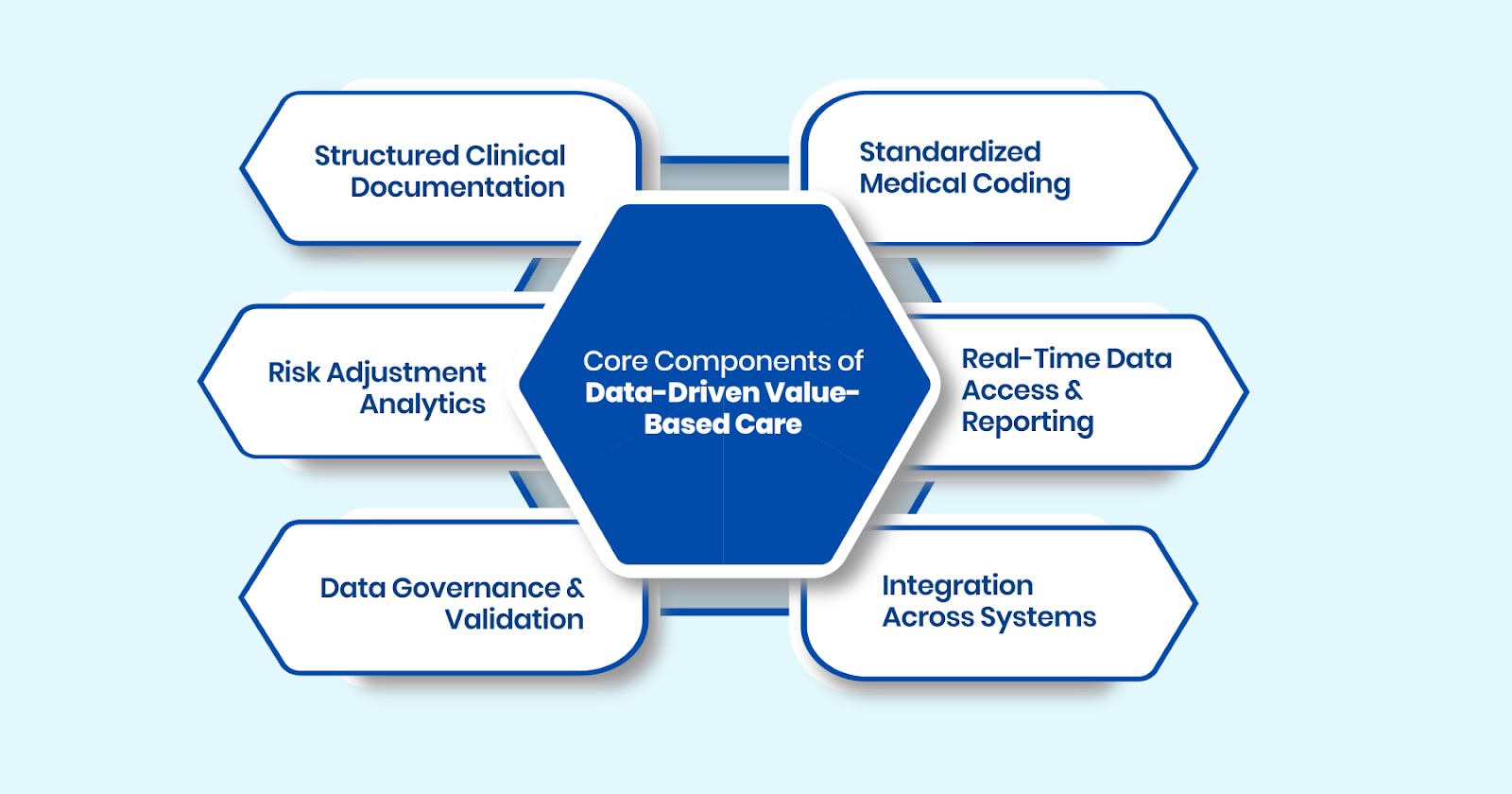
1. Structured Clinical Documentation
Accurate, standardized documentation forms the backbone of data-driven care.
- Captures diagnoses, procedures, SDOH, and patient-reported outcomes using consistent templates
- Supports audits, coding accuracy, and quality reporting
2. Standardized Medical Coding
Clinical encounters must be translated into billable codes (ICD-10, CPT, HCC) to reflect care complexity.
- Ensures alignment with payer-specific reimbursement models
- Minimizes claim denials due to undercoding or errors
3. Risk Adjustment Analytics
Risk models ensure fair compensation for treating high-complexity patients.
- Identifies chronic conditions and comorbidities for accurate RAF scoring
- Aids in resource allocation and long-term care planning
4. Real-Time Data Access and Reporting
Timely insights support proactive interventions.
- Dashboards highlight care gaps, quality metrics, and coding trends
- Enables performance monitoring at provider, team, or facility levels
5. Data Governance and Validation
Reliable outcomes depend on trustworthy data.
- Establishes traceability, audit-readiness, and accountability
- Detects inconsistencies before they impact compliance or reimbursement
6. Integration Across Systems
Interoperability ensures seamless data exchange across platforms.
- Connects EHRs, billing tools, labs, and payers to eliminate silos
- Streamlines workflows by linking clinical documentation to administrative processes
Challenges in Data-Driven Value-Based Care
Even as healthcare organizations invest in value-based initiatives, many encounter foundational issues that prevent data from becoming a truly actionable asset. These challenges are often not purely technical but tied to people, processes, and evolving policy environments.
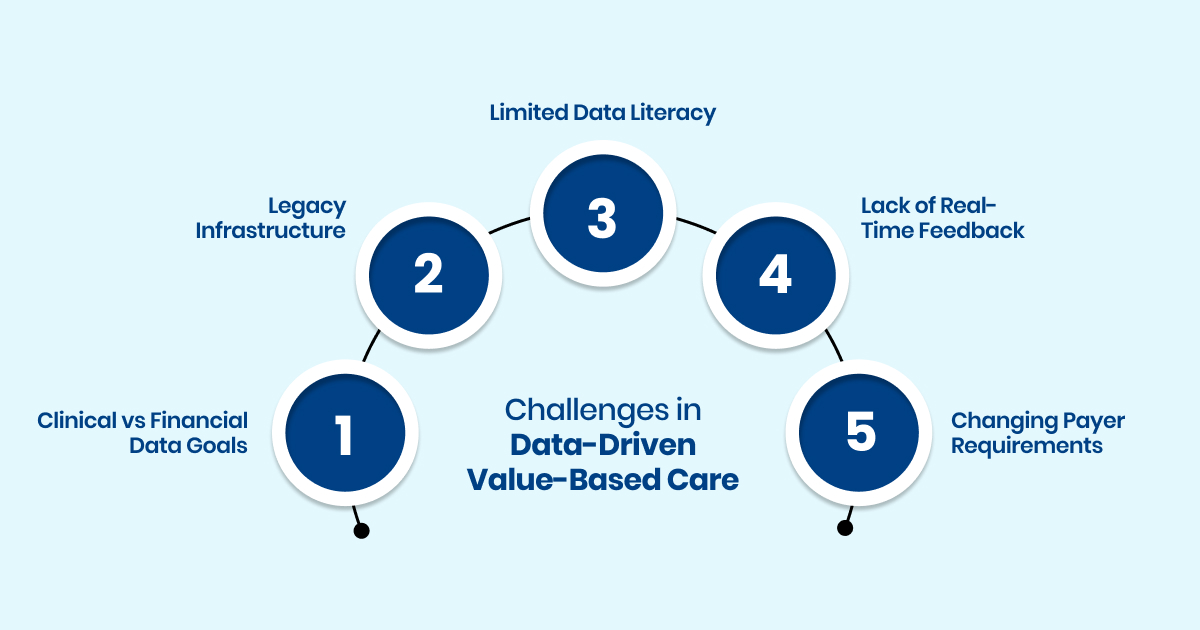
1. Misalignment Between Clinical and Financial Data Goals
Clinical teams often focus on care delivery and outcomes. Financial teams prioritize reimbursement and compliance. Without shared metrics or integrated workflows, data collected for one purpose may not support the needs of the other.
- For example, a care manager might document social risk factors in free text. If this information is not coded properly, it cannot be used for risk scoring or claims.
- This disconnect leads to underutilized data and missed reimbursement opportunities.
2. Legacy Infrastructure That Limits Interoperability
Many healthcare systems still use fragmented, on-premise software that does not support modern data exchange standards such as FHIR or real-time API connections.
- As a result, integrating EHRs with billing tools, coding engines, or risk platforms often requires manual workarounds.
- This slows innovation and increases reliance on outdated batch processes.
3. Limited Data Literacy Across Non-Technical Teams
Clinical and administrative staff work closely with data but often lack training in how their documentation impacts coding, quality metrics, or reimbursement.
- Teams may not realize how incomplete records affect value-based payments or audit outcomes.
- This lack of awareness leads to inconsistent data entry and lower adoption of data-driven workflows.
4. Absence of Real-Time Feedback Loops
Many organizations identify documentation or coding gaps only after a claim is denied or flagged during an audit, when it is too late to fix the issue.
- Without built-in alerts or validation tools, small issues such as missing timestamps or unsupported diagnoses go unnoticed.
- Over time, these errors accumulate, increasing financial and compliance risk.
5. Rapidly Changing Payer Requirements
Performance benchmarks, risk models, and coding rules are frequently updated by payers. Organizations without systems in place to track these changes often struggle to stay aligned.
- Delays in applying coding updates or payer-specific policies can result in submission errors and lower reimbursements.
- Smaller practices, in particular, may lack the resources to manage these updates consistently.
How Technology Supports Data-Driven Value-Based Care
Technology plays a critical role in making data usable, accessible, and actionable. While clinical documentation and coding practices form the foundation, it’s modern technology that helps scale, standardize, and streamline those efforts across the care continuum.
AI-Powered Coding Assistance
Platforms like RapidClaims use machine learning and natural language processing (NLP) to interpret clinical notes and recommend codes in real time.
- Surfaces potential diagnosis and procedure codes from unstructured documentation
- Helps coders catch missing details, reducing the likelihood of undercoding or denials
- Increases throughput without sacrificing coding quality
Workflow-Integrated Compliance Tools
Built-in validation systems and compliance logic can prevent costly errors before claims are submitted.
- Applies payer-specific rules, coding guidelines, and local coverage determinations automatically
- Surfaces documentation gaps early, reducing rework and improving first-pass claim acceptance
- Helps teams stay aligned with evolving regulatory frameworks without constant manual updates
Real-Time Quality and Performance Dashboards
Interactive dashboards make it easier for clinical, coding, and revenue teams to stay informed and aligned.
- Tracks key performance indicators (KPIs) like quality scores, open care gaps, and documentation trends
- Enables team leads to monitor performance at the provider or department level
- Helps organizations adapt quickly if benchmarks are not being met
Interoperability Enablers
APIs and integration frameworks (such as HL7 and FHIR) ensure systems can exchange information seamlessly.
- Connects EHRs, billing software, and third-party coding tools to eliminate data silos
- Enables consistent data formatting across platforms, improving continuity of care
- Supports secure data sharing for value-based contracts that involve multiple stakeholders
Scalable Automation for High-Volume Environments
For organizations dealing with thousands of patient records, automation can help maintain speed without compromising accuracy.
- Automatically processes repetitive or rules-based coding tasks
- Ensures timely data flow for reporting, population health tracking, and reimbursement cycles
- Frees up staff to focus on higher-value activities like exception handling and quality improvement
Practical Applications of Data in Healthcare Workflows
In a value-based environment, data must move beyond dashboards and reports. It needs to inform everyday decisions across clinical, administrative, and financial functions. Here’s how that plays out in real workflows:
- Proactive Risk Identification: Analyzing patient history, comorbidities, and social determinants helps identify high-risk individuals early, enabling timely intervention and better care planning.
- Preventive Care Management: Structured data allows organizations to track missed screenings, follow-ups, and immunizations; closing care gaps that impact quality scores and patient outcomes.
- Seamless Care Coordination: Unified data access across providers ensures continuity, reduces duplication, and supports smooth transitions from primary to specialty or post-acute care.
- Documentation-Driven Reimbursement: Accurate and complete documentation, when paired with standardized coding, ensures that reimbursement reflects the true complexity and scope of care provided.
- Operational Agility: Real-time insights into provider performance, patient volumes, and coding patterns help administrators adjust workflows, resources, and priorities as needed.
What This Means for Healthcare Teams
A data-driven approach to value-based care doesn’t just change systems, it changes how people work. From clinicians to coders to administrators, each role plays a part in translating data into measurable outcomes.
For Clinicians
- Gain visibility into patient history, risk profiles, and open care gaps during the encounter
- Make treatment decisions backed by real-time, evidence-based insights
- Spend less time on administrative follow-ups due to improved documentation workflows
For Medical Coders and Documentation Specialists
- Work with structured, AI-assisted documentation that reduces ambiguity
- Focus on exception handling and high-complexity cases rather than manual lookups
- Improve accuracy and reduce denials with automated rule validation
For Revenue Cycle and Compliance Teams
- Monitor claim readiness, coding completeness, and documentation compliance in real time
- Reduce delays in accounts receivable through faster, cleaner submissions
- Prepare confidently for audits with traceable, well-documented coding logic
For Operational and Quality Leads
- Track organizational performance across metrics that impact both care and reimbursement
- Use data trends to inform process improvements and resource planning
- Align teams around shared goals with transparent, role-specific insights
Conclusion
Value-based care promises better outcomes, but achieving that promise depends on how well healthcare organizations use their data. From risk adjustment to care coordination to reimbursement, every part of the value-based model relies on clean, complete, and timely information.
Organizations that invest in structured documentation, coding accuracy, and real-time insights are better equipped to meet quality benchmarks, reduce denials, and improve patient outcomes, without overburdening their teams.
Want to reduce denials, close risk gaps, and drive stronger VBC revenue? See how RapidClaims powers smarter, faster documentation and coding workflows.. Request a demo to get started.
FAQs
Q. What is data-driven value-based care?
Ans: Data-driven value-based care is a healthcare model where clinical and operational decisions are guided by structured data. This approach ties reimbursement to patient outcomes rather than service volume, requiring accurate documentation, risk scoring, and performance tracking.
Q. Why is data important in value-based care?
Ans: Data enables providers to measure outcomes, stratify risk, track quality metrics, and comply with payer requirements. Without clean and timely data, it is difficult to qualify for performance-based incentives or avoid revenue losses.
Q. How does poor data quality affect reimbursement?
Ans: Inaccurate or incomplete data can lead to undercoding, missed risk adjustment opportunities, claim denials, and audit penalties. Poor data also skews quality reporting, which can negatively impact incentive payments.
Q. What role do AI tools play in supporting value-based care?
Ans: AI tools automate coding, validate documentation, and flag compliance issues in real time. They help healthcare teams scale their operations, reduce manual rework, and maintain accuracy across high-volume environments.
Q. What are the biggest barriers to implementing data-driven strategies in healthcare?
Ans: Key challenges include fragmented systems, legacy infrastructure, lack of data literacy among staff, and constant changes in payer requirements. These make it difficult to unify and act on data effectively.
.png)
Ayeesha Siddiqua
Ayeesha Siddiqua is a highly experienced medical coding professional with 22 years of expertise in E/M Outpatient, Radiology, and Interventional Radiology (IVR), ensuring coding accuracy, regulatory compliance, and optimized reimbursements at RapidClaims.
Latest Post
expert insights with our carefully curated weekly updates
Related Post
Top Products

%201.png)

.jpg)






