.webp)
RapidClaims Healthcare Coverage: Industry Recognition and Real-World Impact

Every healthcare leader wants the same three things from their revenue cycle: accuracy, speed, and predictability. Yet hospitals across the United States lose nearly $262 billion each year due to coding inefficiencies and claim denials. These losses strain margins, delay reimbursements, and limit patient care investments.
This year, leading healthcare publications and research organizations spotlighted RapidClaims for solving these challenges. From Becker’s Hospital Review to Frost & Sullivan and Black Book, the industry’s most trusted evaluators recognize RapidClaims as a proven platform for accuracy, compliance, and efficiency.
Key Takeaways
- Becker’s Hospital Review highlighted RapidClaims for accuracy, speed, and efficiency in coding operations.
- Frost & Sullivan recognized RapidClaims for leadership in healthcare IT innovation and measurable customer outcomes.
- Black Book ranked RapidClaims among the top vendors in 2025 for user satisfaction and ROI.
- Hospitals and physician networks trust RapidClaims to improve accuracy and compliance across more than 25 specialties.
Table of Contents:
- RapidClaims Healthcare Coverage: Industry Recognition and Real-World Impact
- Becker’s Hospital Review: RapidClaims Sets New Standards in Coding Accuracy
- Frost & Sullivan Recognizes RapidClaims for Healthcare IT Innovation
- Black Book 2025: RapidClaims Ranked Top Vendor for RCM Automation
- Expanding Recognition: Adoption Across Hospitals and Specialties
- What These Recognitions Mean for Healthcare Providers
- Case Examples of Industry Impact
- Healthcare Leaders’ Perspectives
- Conclusion: Continuous Improvement and Commitment to Clients
Becker’s Hospital Review: RapidClaims Sets New Standards in Coding Accuracy
When Becker’s Hospital Review examined the causes of revenue cycle losses, one factor stood out: the time and resources hospitals spend correcting coding errors.
Becker’s highlighted RapidClaims for helping health systems reclaim revenue with reliable, consistent, and audit-ready coding.
The publication underscored how RapidClaims combines accuracy, compliance, and operational speed to simplify complex coding workflows.
Becker’s analysis positioned the company as a trusted partner for organizations modernizing their revenue cycle processes.
Highlights from Becker’s Coverage
Becker’s described RapidClaims as a driver of measurable, sustainable improvement across healthcare finance operations. The coverage reinforced that improved coding isn’t only a compliance need, it’s a revenue recovery strategy.
Read the full article on Becker’s here.
Frost & Sullivan Recognizes RapidClaims for Healthcare IT Innovation
Frost & Sullivan awarded RapidClaims the 2025 North American Healthcare IT Software and Services Technology Innovation Leadership Award for excellence in RCM automation. The recognition highlights RapidClaims’ innovation in accuracy optimization, scalability, and user impact.
You can see how this recognition aligns with what many healthcare leaders already experience: consistent results, high performance, and measurable efficiency gains.
Frost & Sullivan Evaluation Summary
Frost & Sullivan’s evaluation confirmed RapidClaims’ position as a technology partner focused on real-world results. Hospitals using the platform report higher coding throughput and smoother integrations with existing billing systems.
You can explore Frost & Sullivan’s announcement here.
Black Book 2025: RapidClaims Ranked Top Vendor for RCM Automation
Independent evaluations often tell the clearest story. The Black Book 2025 Vendor Satisfaction Ratings placed RapidClaims among the top healthcare IT platforms for reliability, accuracy, and user satisfaction.
Alt text:Black Book 2025: RapidClaims Ranked Top Vendor for RCM Automation
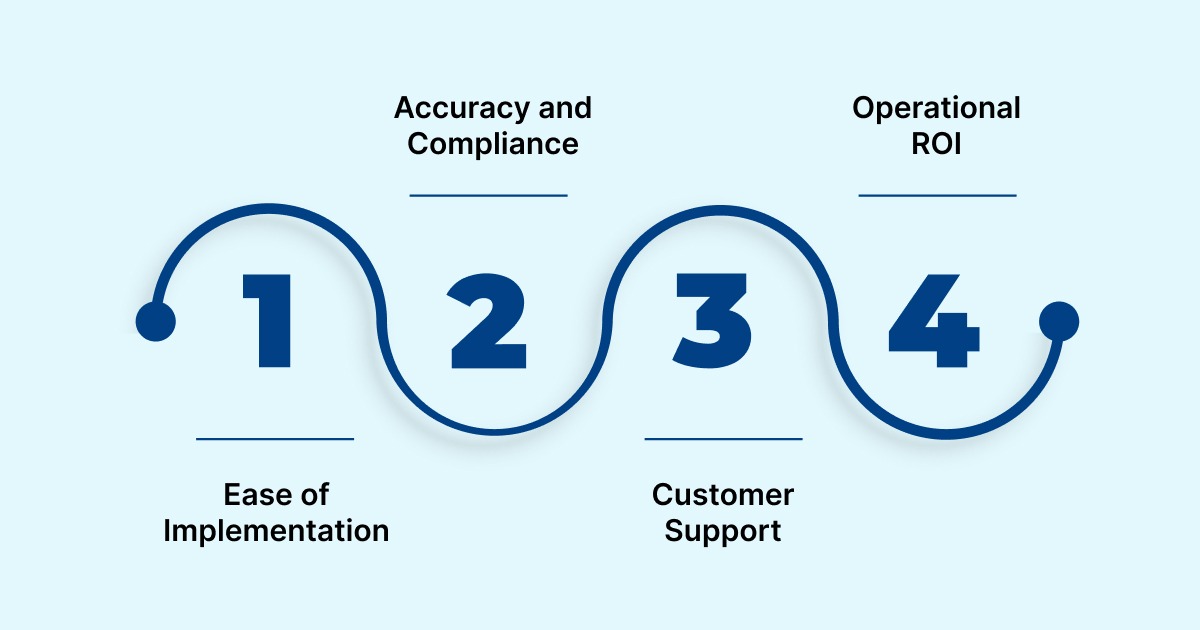
Healthcare leaders, billing teams, and compliance officers rated RapidClaims highest across multiple categories, including ease of implementation, operational ROI, and customer support quality.
What Black Book Found
- Ease of Implementation: RapidClaims scored highest for deployment speed and integration simplicity.
- Accuracy and Compliance: Recognized for consistent adherence to ICD-10 and payer policies.
- Customer Support: Rated exceptional for post-go-live service and response time.
- Operational ROI: Users reported significant reductions in time-to-code and denial volume.
You can review Black Book’s summary on Finance Yahoo.
These findings reinforce what hospitals expect from their technology partners: solutions that deliver clear outcomes without complexity.
Expanding Recognition: Adoption Across Hospitals and Specialties
Becker’s Hospital Review also featured RapidClaims’ expansion to 25+ medical specialties, confirming the platform’s ability to maintain accuracy and compliance across diverse service lines. This breadth shows adaptability; your coding teams can manage a variety of chart types through one consistent system.
Hospitals, physician groups, and medical billing companies use RapidClaims to streamline workflows, improve claim turnaround, and reduce denials in complex specialties.
What Healthcare Teams Report
- Hospital Administrators: Improved coding efficiency and measurable revenue uplift.
- Coders: Less time spent on manual rework and higher accuracy per chart.
- Physicians: Clearer documentation feedback and reduced billing friction.
- Finance Leaders: Steadier cash flow and fewer payer rejections.
These results demonstrate that RapidClaims works at scale, supporting healthcare systems that manage thousands of charts per day.
Read Becker’s coverage on specialty growth here.
What These Recognitions Mean for Healthcare Providers
When respected analysts and healthcare media share the same message, it confirms that the results are real. Each recognition, Becker’s Hospital Review, Frost & Sullivan, and Black Book, tells a unified story of reliability and measurable value.

Alt text:What These Recognitions Mean for Healthcare Providers
You rely on technology that protects margins, reduces administrative load, and supports compliance. RapidClaims consistently delivers these outcomes. The following points show what these recognitions translate to in practice:
- Higher coding accuracy improves your audit readiness and reimbursement reliability.
- Lower denial rates strengthen your revenue cycle and create predictable financial performance.
- Faster implementations let your teams work productively without long IT projects.
- Lower costs allow more budget for clinical operations and patient initiatives.
- Specialty scalability ensures consistency from primary care to complex inpatient services.
When your organization invests in a platform trusted by independent evaluators, you gain confidence in every claim submitted.
Case Examples of Industry Impact
RapidClaims’ industry coverage isn’t limited to press mentions; hospitals and physician networks already see measurable improvement. These outcomes show how consistent performance creates long-term value for coding and finance leaders.
Example 1: Large Physician Group
A 120-provider practice faced recurring denials and high administrative costs due to manual coding errors.
After implementing RapidClaims, the group reduced coding-related denials by 70% and cut operational costs by 30%. The coding team processed more charts per day while maintaining full compliance.
Example 2: Multispecialty Hospital Network
A regional hospital system integrated RapidClaims across 15 departments, including radiology, emergency care, and obstetrics. The results included 96% coding accuracy, a 25% faster A/R cycle, and reduced staff overtime.
Hospital executives reported improved morale among coders due to lower error correction workloads.
These examples show what Becker’s, Frost & Sullivan, and Black Book observed: measurable performance that directly supports financial stability and patient care delivery.
Healthcare Leaders’ Perspectives
Healthcare executives and operations leaders share similar views on the platform’s effectiveness. Their feedback highlights how real-world experience matches the industry recognition.
"RapidClaims has transformed our medical coding operations. Their AI-driven automation has reduced our claim denials by nearly half, allowing our coders to focus on complex cases instead of routine tasks."
- CEO, Physician Group (120 Providers)
"AI is making human coders more efficient, allowing them to focus on decision-making rather than data entry. RapidClaims’ automation has been a game-changer for our team."
- Sachin Jain, President & CEO, Scan Health
"Medical coding is one of the biggest challenges we face as physicians. The automation provided by RapidClaims allows us to spend more time with patients instead of dealing with billing issues."
- Dr. Chethan Satya, Pediatric Thoracic Surgeon
These testimonials confirm what the awards validate: consistent improvement across accuracy, compliance, and cost control.
Conclusion: Continuous Improvement and Commitment to Clients
Recognition brings visibility, but continuous improvement builds longevity. RapidClaims keeps updating its platform to stay aligned with new payer regulations, ICD-10 revisions, and E/M code guidelines.
You benefit from:
- Weekly updates that refresh payer rule sets automatically.
- Real-time visibility into claim performance metrics.
- Audit-ready records accessible through secure dashboards.
- Dedicated support during policy or compliance transitions.
The focus on reliability and client success drives ongoing recognition from healthcare institutions.
As rules evolve, RapidClaims ensures your organization stays ahead of regulatory and financial challenges.
Explore how RapidClaims can help your organization achieve higher accuracy, faster payments, and stronger compliance.
Latest Post
- RapidClaims Healthcare Coverage: Industry Recognition and Real-World Impact
%201.png)



