Revolutionizing Healthcare: AI and ML Strategies for Revenue Cycle Innovation

Ever wondered how much U.S. hospitals spend on administrative costs each year? Medicare Cost Reports from 5,639 hospitals show expenses reached $166.1 billion, accounting for 17% of total spending and creating tighter margins for revenue cycle teams.
These rising costs and frequent payer policy changes put RCM professionals under pressure, resulting in slower reimbursements, increased workloads, and heightened compliance risks. AI and ML in the revenue cycle can help automate processes, enhance accuracy, and reduce denials, making operations more efficient and cost-effective.
In this blog, you’ll explore how AI and ML revenue cycle enhancements improve healthcare operations, address challenges, and offer strategies for overcoming obstacles.
TL;DR (Key Takeaway)
- AI/ML Automation: Automates coding, documentation, claim submission, denial management, and payment posting.
- Error Reduction & Compliance: Predictive models and NLP prevent denials, detect revenue leakage, and improve audit transparency.
- Integrated Platforms: Solutions like RapidClaims combine AI automation, smart edits, managed denial recovery, and real-time payer feedback.
- Adoption Challenges: Data quality, model transparency, regulatory compliance, payer rules, and staff resistance require clear mitigation strategies.
- Future Potential: Enables fully automated revenue cycles, AI-assisted documentation, embedded compliance, and broader adoption by smaller providers.
Table of Contents:
- What is Revenue Cycle Management (RCM)?
- Key Challenges in Traditional Revenue Cycle Management
- How AI and ML Streamline Healthcare Revenue Cycle Management?
- Key Use Cases & their Audit / Compliance Implications
- Overcoming Barriers to AI and ML Adoption in RCM
- What the Future Holds for AI and ML in Healthcare RCM?
- Conclusion
- Frequently Asked Questions (FAQs)
What is Revenue Cycle Management (RCM)?
Revenue Cycle Management (RCM) in healthcare oversees all financial processes linked to patient care. This includes pre-registration, insurance verification, clinical documentation, coding, claim submission, denial handling, payment posting, and patient billing. Its goal is to ensure accurate and timely reimbursement while maintaining regulatory compliance.
RCM is challenging due to changing payer rules, Medicare and Medicaid guidelines, and compliance obligations such as HIPAA and the False Claims Act. Missed charges, underpayments, and claim denials directly lower revenue; therefore, healthcare organizations require precise oversight and well-designed processes to prevent losses.
Now, let’s explore the challenges of traditional revenue cycle management to understand why AI and ML have become essential solutions in healthcare.
Key Challenges in Traditional Revenue Cycle Management
Despite significant investments in EHRs, practice management systems, and billing platforms, many healthcare providers continue to face persistent inefficiencies in revenue cycle management:

Alt text:Key Challenges in Traditional Revenue Cycle Management
- High Denial Rates And Rework Burden: Claims frequently fail due to coding errors, missing documentation, eligibility issues, or payer-specific rules, requiring repeated corrections.
- Revenue Leakage and Undercoding: Clinicians or coders may overlook billable services, or documentation may not fully justify the highest reimbursable level, resulting in financial losses.
- Fragmented Systems and Isolated Data: Clinical, billing, and payer data often reside in disconnected systems, causing duplication, mapping errors, and delays in processing.
- Manual Workflows and Human Error: Steps such as documentation review, editing, and appeals remain labor-intensive, inconsistent, and prone to mistakes.
- Limited Forecast Visibility and Analytics: Traditional RCM relies on lagging indicators, spreadsheets, and manual dashboards, making it difficult to detect trends or anomalies early.
- Compliance Risk: Close interaction with regulatory rules means that insufficient documentation, lack of audit trails, or flawed manual overrides can expose organizations to penalties and risk.
Also Read: From Chaos to Clarity: How AI in Medical Coding Enhances Accuracy
These ongoing challenges slow reimbursements and drive up costs, so let’s understand why AI and ML have become vital for modernizing the revenue cycle.
How AI and ML Streamline Healthcare Revenue Cycle Management?
Artificial Intelligence (AI) and Machine Learning (ML) bring predictive, pattern-recognition, and natural language processing (NLP) capabilities to address manual, error-prone tasks in RCM. Here’s how AI/ML reshapes key revenue cycle management stages:
1. Eligibility & Insurance Verification
AI ensures accurate verification of patient coverage before services are rendered, reducing denials and administrative delays. This stage is proactive, focused on preventing issues before claims are generated.
- Automatically queries payer databases in real time.
- Detects lapses, inconsistencies, or high-risk patient coverage.
- Predicts potential eligibility changes based on historical data.
- Minimizes claim rejections due to eligibility errors.
2. Clinical Documentation & Charge Capture
AI leverages NLP and generative models to extract billable services from physician notes, lab results, and imaging reports. The goal is to maximize revenue capture before coding.
- Identifies missing or incomplete billable services.
- Suggests appropriate CPT, ICD-10, or HCPCS codes in real time.
- Prompts physicians for clarifications to ensure documentation supports billing.
- Maintains audit-ready records for compliance and review.
3. Coding & Claim Scrubbing
ML models analyze historical claims and payer behavior to optimize coding accuracy during claim preparation, ensuring compliance and reducing submission errors.
- Detects missing modifiers, conflicting codes, or non-compliant combinations.
- Performs multi-layered “smart scrubbing” before submission.
- Ensures alignment with current payer-specific coding rules.
- Reduces human error and downstream rework.
4. Pre-Submission Denial Prediction
AI evaluates claims for the likelihood of denial proactively, enabling corrections before submission to prevent potential denials.
- Scores claims based on historical denial patterns and payer rules.
- Flags high-risk claims for human review or automated adjustment.
- Bundles necessary documentation to improve approval chances.
- Reduces rejected claims and accelerates revenue flow.
5. Denial Handling & Appeals
AI automates the reactive handling of denied claims, identifying root causes and streamlining the appeals process.
- Categorizes denials by cause and severity.
- Generates payer-specific appeal letters.
- Routes complex cases to appropriate teams efficiently.
- Feeds outcomes back into predictive models to improve future claim approvals.
6. Payment Posting & Reconciliation
AI automates operational processes related to matching payments to claims and detecting discrepancies, ensuring accurate revenue posting.
- Parses ERAs/EOBs and reconciles payments to claims.
- Flags underpayments, short-pays, or mismatches.
- Initiates follow-up actions automatically.
- Improves the accuracy of cash posting and reduces manual workload.
7. Patient Billing & Collections
Predictive AI models personalize patient engagement and optimize collections, focusing on front-end and patient-facing revenue capture.
- Assesses patients’ likelihood to pay and segments communication.
- Delivers personalized messages via text, portal, email, or calls.
- Suggests tailored repayment plans based on patient behavior.
- Enhances collections while maintaining patient satisfaction.
8. Forecasting, Analytics & Audit Support
AI provides strategic, organization-wide insights by analyzing trends, detecting anomalies, and supporting risk-based audits.
- Monitors claims, denials, and payment patterns for anomalies and discrepancies.
- Forecasts cash flow and identifies operational bottlenecks.
- Supports internal audit with risk-based sampling and real-time alerts.
- Enables leadership to make data-driven decisions on resource allocation, staffing, and policy improvements.
By embedding AI/ML across all stages, the revenue cycle becomes more proactive, adaptive, and resilient.
In practice, platforms like RapidClaims illustrate this transformation. Their AI-powered Rapid Agents, RapidCode, RapidCDI, and RapidScrub, aggregate clinical and RCM data, automate coding, edits, and appeals, and support compliance-ready workflows. This improves coding accuracy, optimizes HCC capture, reduces denials, and accelerates claim processing, turning the theoretical benefits of AI/ML into measurable operational results.
Key Use Cases & their Audit / Compliance Implications
AI and ML enhance the revenue cycle by embedding traceability and accountability into every step of the process. This transparency allows auditors and compliance teams to monitor operations, verify adherence to regulations, and maintain internal controls.
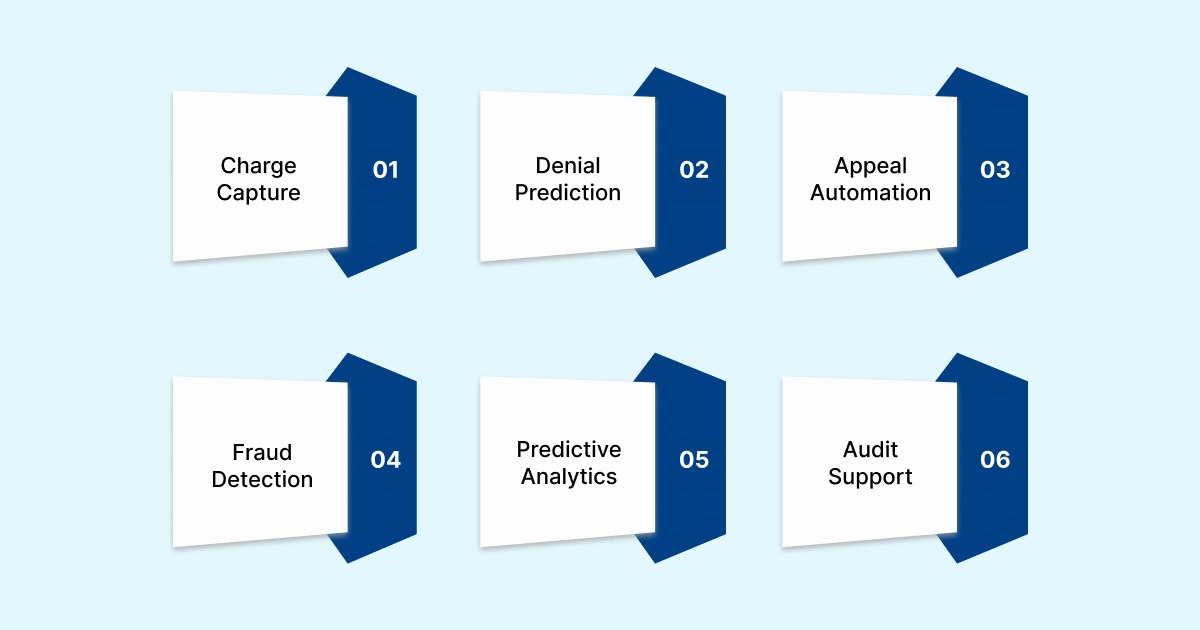
Alt text:Key Use Cases & their Audit / Compliance Implications
Below are a few use cases that show how AI/ML enhances key RCM functions:
1. Charge Capture and Revenue Leakage Prevention
Use case: Hospitals can lose 1–3% of net patient revenue due to missed or undercaptured charges. AI tools analyze clinical documentation, compare expected charge patterns, and flag likely missing charges before submission. Systems can cross-check physician orders, lab results, imaging, and documentation trends to surface underbilled services.
Audit/compliance lens:
- Audit teams must validate the AI’s logic, including how expected charges are defined, reference datasets used, and thresholds for alerts.
- The risk of overbilling exists if the AI suggests adding services that are not fully documented; auditors must confirm clinical necessity.
- Periodic sampling of flagged versus accepted charges ensures adherence to payer rules and minimizes audit exposure.
2. Denial Prediction and Preventive Edits
Use case: AI and ML models trained on historical claims can detect patterns that lead to denials, such as missing modifiers, mismatched DRGs, or insufficient documentation. Systems can alert, block, or suggest corrections for high-risk claims before submission, and may auto-generate attachments or appeal drafts.
Audit/compliance lens:
- Auditors should review claims flagged but overridden by staff to ensure overrides are justified.
- Analysis of submitted claims flagged for denial can reveal model tuning gaps or user errors.
- Model performance must be regularly monitored for drift; retraining logs, version control, and validation metrics should be maintained accordingly.
3. Appeal Automation and Root Cause Clustering
Use case: AI clusters similar denials, identifies root causes, and generates appeal templates. Systems learn over time which appeals succeed and refine future submissions.
Audit/compliance lens:
- Auditors should review appeal letters to confirm clinical accuracy and compliance with documentation standards.
- Generic appeals sent indiscriminately must be controlled; high-value claims should undergo oversight.
- Appeal success rates should be closely monitored, with adjustments made if trends indicate a decline in performance.
4. Fraud, Waste, and Abuse Detection
Use case: ML models detect anomalous billing, duplicates, upcoding, or policy violations by comparing patterns against peer data or historical claims. Studies have shown ML can achieve over 98.8% accuracy in detecting Medicare fraud.
Audit/compliance lens:
- AI-detected outliers should be treated as high-risk for review.
- Explainability is critical: auditors must understand the features that trigger anomaly scores and the corresponding threshold settings.
- Regulatory compliance requires traceable interventions, including logs and justifications, for all AI actions.
5. Predictive Analytics and Financial Forecasting
Use case: AI models can forecast revenue, cash flow gaps, and resource needs by analyzing claim volumes, payer patterns, seasonal trends, and denials. Forecasting is more accurate than static models and supports operational planning.
Audit/compliance lens:
- Forecast models should be backtested against actual results, with discrepancies explained.
- Auditors may validate assumptions, inputs, and stress-test forecasts under adverse scenarios to ensure accuracy.
- The integrity of models is essential if their outputs influence budgeting or performance targets.
6. Audit Support and Integrity Sampling
Use case: AI assists internal audit by generating risk-based samples, flagging high-dollar transactions, and identifying unusual trends. It acts as an additional layer of monitoring revenue data.
Audit/compliance lens:
- AI recommendations should be advisory; human judgment and validation remain essential.
- Controls must define who authorizes sampling logic and how frequently it is refreshed.
- Transparency is key: logs, model versions, thresholds, and sampling criteria must be fully documented.
A platform like RapidClaims shows how AI/ML can accelerate revenue capture while maintaining compliance. Its RapidRecovery module combines AI insights with expert-managed denial recovery, overturning claims in under 30 days on a contingency basis. With real-time policy alerts, smart edits, and continuous payer feedback, improve A/R speed, reduce collection costs, and deliver measurable ROI.
Now, let’s examine the key barriers to AI and ML adoption in the revenue cycle and ways to address them.
Overcoming Barriers to AI and ML Adoption in RCM
Introducing AI/ML into your RCM is a significant undertaking. Below are common barriers and suggested mitigation strategies:
1. Poor Data Quality and Isolated Systems: AI models depend on clean, well-structured data. Legacy systems, disparate EHRs and billing platforms, nonstandard mappings, and unstructured clinical notes hinder accuracy.
- Mitigation: Establish robust data governance, harmonize terminologies (ICD, CPT, SNOMED), build clean ingestion pipelines, preprocess and standardize data, and initiate integration with core systems (EHR and billing).
2. Explainability and Auditability of Models: Deep learning or opaque models may offer predictive power but lack interpretability, which is problematic for compliance and audits.
- Mitigation: Favor explainable AI (XAI) models or incorporate interpretability layers (e.g., SHAP, LIME). Maintain version control, logs, feature attribution, and documentation to enable auditors and compliance officers to trace decisions.
3. Model Drift and Evolving Payer Rules: Payer policies, coding guidelines, reimbursement rules, and clinical practices evolve. Models degrade over time.
- Mitigation: Continuously monitor model accuracy, schedule retraining, validate performance, and incorporate feedback loops.
4. Regulatory, Privacy, and Compliance Risks: AI systems work with PHI, claims data, and sensitive financial records; oversight is necessary to avoid HIPAA violations, unintentional bias, or contractual risk.
- Mitigation: Conduct HIPAA risk assessments, deploy role-based access controls, audit trails, encryption, data minimization, and adhere to vendor contracts with compliance guarantees.
5. Staff Adoption and Change Management
Coders, auditors, and billing staff may resist AI, fearing job loss or distrusting the “black box” nature of its suggestions. Overreliance or misuse may occur.
- Mitigation: Engage stakeholders early, pilot small use cases, provide training, implement human-in-the-loop workflows, and demonstrate clear benefits.
Also Read: AI and Automation in Denial Management for Healthcare
By proactively addressing these barriers, health systems increase their chances of deploying AI/ML successfully without undue risk.
What the Future Holds for AI and ML in Healthcare RCM?
As healthcare revenue cycles grow increasingly challenging, AI and ML are poised to shift from supporting tasks to actively predicting issues and embedding compliance. The following are the near-future trends that highlight how intelligent automation will transform efficiency, accuracy, and decision-making in RCM:

Alt text:What the Future Holds for AI and ML in Healthcare RCM?
- End-to-End Autonomous Revenue Cycle Orchestration: AI systems will manage eligibility, documentation, coding, submission, denials, appeals, reconciliation, and collections in a unified engine, reducing manual intervention.
- Generative AI for Documentation and Appeals: Generative models will assist in drafting clinical documentation, appeal narratives, and patient communications, while ensuring compliance with coding and regulatory requirements.
- Real-Time Payer-Provider Feedback Loops: AI platforms will continuously learn from live payer responses, adjudication patterns, and denial trends, improving predictive accuracy and claim approval rates.
- Embedded Compliance and Guardrails: AI will include built-in audit logs, override rules, policy checks, and error detection to ensure adherence to regulatory standards.
- Broader Adoption Across Smaller Providers: Modular, cost-effective AI tools will make RCM automation accessible to outpatient clinics, speciality groups, and small practices.
These advancements suggest that AI /ML will play a central role in the revenue cycle, improving claims processing, reducing errors, ensuring compliance, and delivering actionable insights for informed decision-making.
Conclusion
Manual revenue cycle processes continue to burden revenue cycle professionals with high administrative costs, slow claim processing, and an increased risk of denials. AI and ML solutions can automate coding, detect errors, and enhance compliance, transforming revenue cycle efficiency.
With platforms like RapidClaims, healthcare organizations can streamline claims processing, reduce denials, and maintain audit readiness while ensuring regulatory compliance. RapidClaims utilizes AI-powered automation across charge capture, denial prediction, and appeals to optimize every step of the revenue cycle.
Ready to increase revenue, reduce denials by 70%, and streamline your healthcare operations? Request a free demo today to see how RapidClaims empowers your staff and optimizes your revenue cycle.
Frequently Asked Questions (FAQs)
1. How can I ensure AI adoption aligns with my organization's specific revenue cycle challenges?
A. To implement AI effectively, first identify your organization’s pain points, such as high claim denials or coding errors. Choose AI solutions that are customizable and can target those specific challenges. Ongoing monitoring and adjustment ensure the technology delivers measurable benefits.
2. I’m concerned about the learning curve for my team. How can I facilitate smooth adoption?
A. Training is critical for successful AI integration. Select platforms with intuitive interfaces and provide step-by-step onboarding sessions. Continuous learning resources, simulations, and support channels help staff adapt quickly without disrupting daily revenue cycle operations.
3. How do I measure the ROI of implementing AI in my revenue cycle?
A. ROI can be measured through metrics like reduction in claim denials, faster reimbursement cycles, improved coding accuracy, and lower administrative costs. Regularly tracking these KPIs helps quantify the financial and operational impact of AI tools on your organization.
4. What are the compliance implications of using AI in healthcare revenue cycles?
A. AI tools must comply with HIPAA, CMS, and other regulatory guidelines. Platforms should provide transparent audit trails, secure data handling, and reporting features. Ensuring regulatory adherence protects patient data and mitigates risk during audits.
5. Can AI tools integrate with my existing EHR and billing systems?
A. Yes, most AI revenue cycle platforms are designed to integrate with major EHR and billing systems using standard APIs and protocols. Proper integration ensures smooth workflow, seamless data exchange, and minimal disruption to existing processes.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products

%201.png)








