Audit-Proof Your Home Health and Hospice: Essential Strategies for Success
Audit-Proof Your Home Health and Hospice: Essential Strategies for Success
Introduction
In the ever-evolving landscape of home health and hospice care, staying compliant and avoiding claim denials is crucial for providers. Recent audit trends reveal persistent challenges in documentation, face-to-face encounters, and medical necessity justification. This comprehensive guide explores these trends and offers strategies for providers to enhance their compliance and documentation practices.
Home Health Audit Trends
Recent data from Centers for Medicare & Medicaid Services (CMS) contractors reveals several key areas where home health providers face claim denials:
1. Medical Necessity for Skilled Nursing Services
Surprisingly, the top reason for denials is related to the medical necessity of skilled nursing services. This shift indicates that auditors are increasingly scrutinizing the actual content of clinical documentation rather than just technical requirements.
2. Face-to-Face Documentation Issues
Despite being in place for over a decade, face-to-face documentation remains a significant challenge. Providers often struggle with: - Missing or incomplete documentation - Untimely encounters - Lack of clear connection between the encounter and the reason for home health services
3. Plan of Care and Certification Problems
Issues with initial certifications, including missing, incomplete, or invalid documentation, continue to be a major cause of denials.
4. Therapy Services Documentation
Even with the removal of therapy thresholds in the Patient-Driven Groupings Model (PDGM), auditors still focus on the medical necessity and complexity of therapy services.
5. Timely Submission of Medical Records
A significant number of denials occur simply because providers fail to submit medical records within the required 45-day timeframe.
Hospice Audit Trends
Hospice providers face their own set of challenges in avoiding claim denials:
1. Terminal Prognosis Documentation
The top reason for hospice denials is insufficient documentation supporting a terminal prognosis of six months or less. This highlights the need for comprehensive, ongoing documentation of the patient's condition and trajectory.
2. Election Statement Issues
Technical problems with hospice election statements, including missing elements or incorrect dates, account for a large portion of denials.
3. Face-to-Face Encounter Requirements
Similar to home health, hospice providers struggle with meeting face-to-face encounter requirements.
4. Timely Submission of Medical Records
As with home health, failure to submit records in a timely manner is a significant issue for hospice providers.
Strategies for Improving Compliance and Reducing Denials
To address these audit trends and minimize the risk of claim denials, providers should focus on the following areas:
1. Enhance Documentation Practices
- Train staff to provide detailed, patient-specific documentation that clearly demonstrates medical necessity - Implement regular internal audits to identify and address documentation gaps - Utilize technology solutions to streamline and improve documentation processes
2. Strengthen Face-to-Face Encounter Processes
- Develop clear protocols for obtaining and documenting face-to-face encounters - Educate referring physicians on the importance of thorough documentation - Implement a system to track and follow up on missing or incomplete face-to-face documentation
3. Improve Physician Collaboration
- Establish strong relationships with referring physicians and educate them on documentation requirements - Develop a process for gentle but persistent follow-up to obtain necessary signatures and documentation - Consider using technology solutions to facilitate easier communication and document exchange with physicians
4. Implement Robust ADR Response Processes
- Create a clear workflow for handling Additional Documentation Requests (ADRs) - Designate specific staff members responsible for managing ADR responses - Set up a system to track deadlines and ensure timely submission of requested documentation
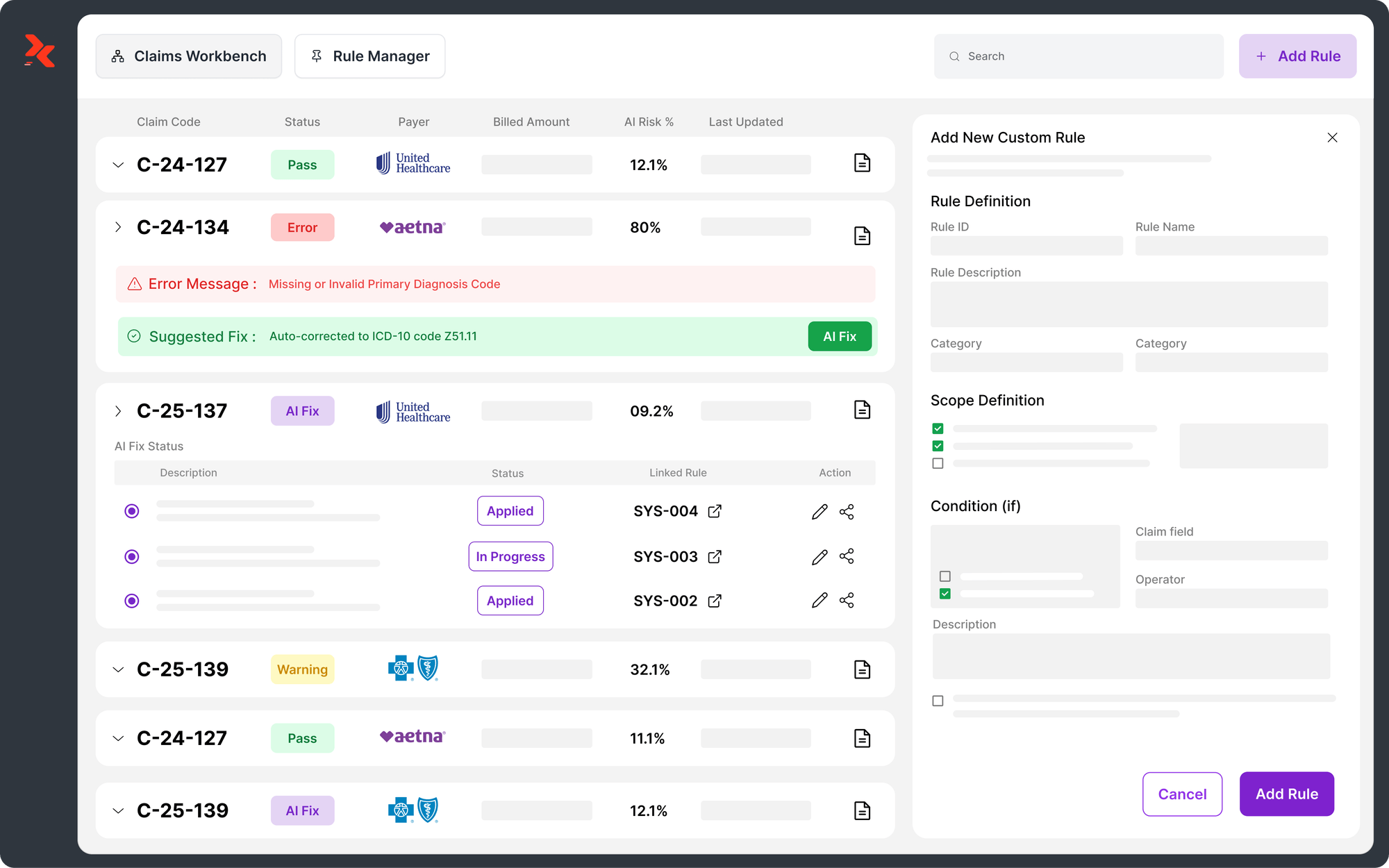
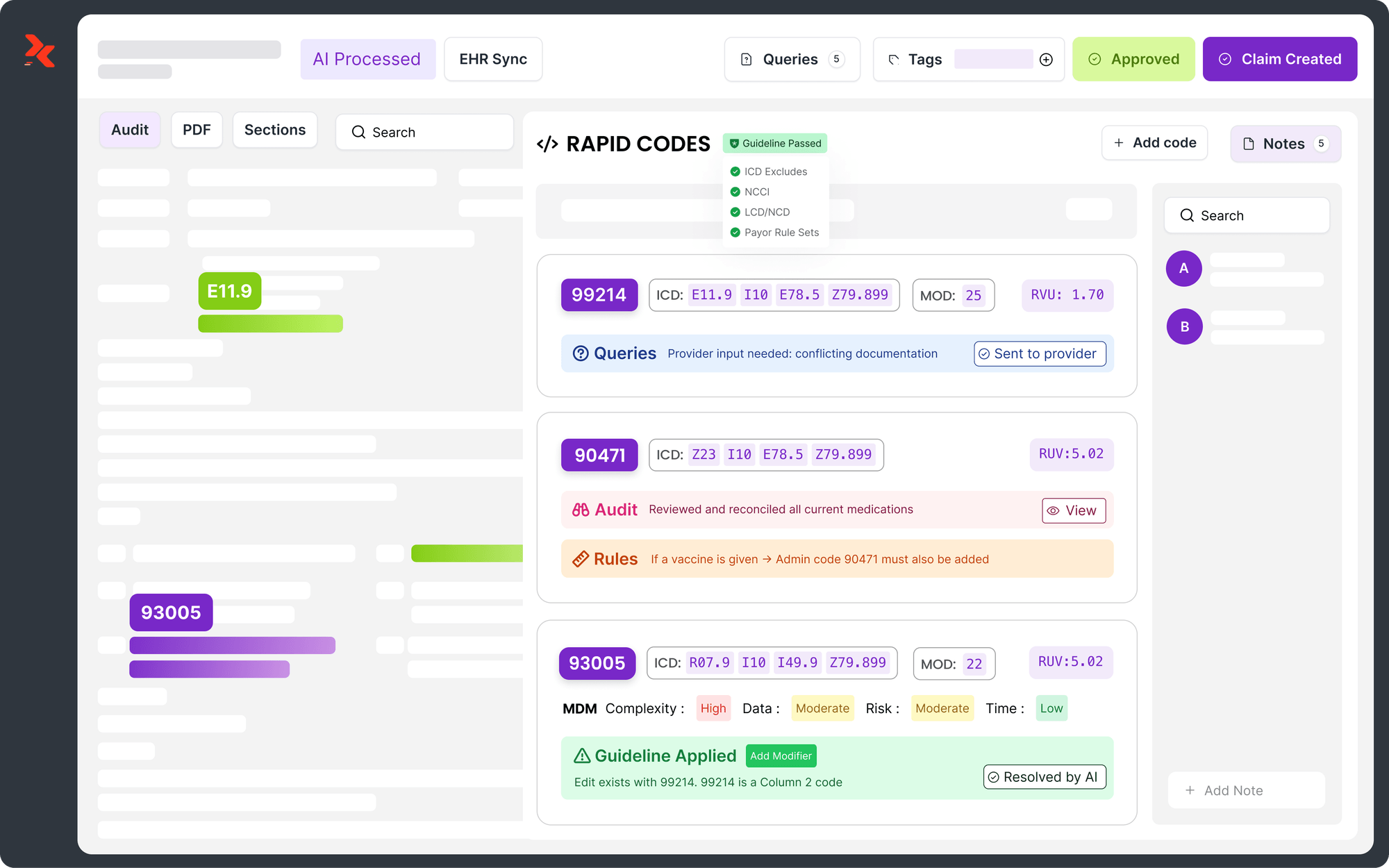
5. Leverage Technology for Compliance
Providers should consider implementing advanced technology solutions, such as RapidClaims, to enhance their coding and documentation processes. RapidClaims' AI-powered coding solution can help: - Streamline the coding process, reducing the risk of errors and omissions - Ensure higher accuracy in translating clinical documentation into precise medical codes - Improve team efficiency by automating routine tasks - Enhance compliance with the latest coding standards - Optimize revenue cycle management by reducing coding-related denials
Conclusion
As audit trends in home health and hospice continue to evolve, providers must stay vigilant and proactive in their compliance efforts. By focusing on comprehensive documentation, improving physician collaboration, and leveraging technology solutions like RapidClaims, providers can significantly reduce their risk of claim denials and ensure they receive appropriate reimbursement for the vital services they provide. Remember, compliance is an ongoing process that requires continuous attention and improvement. By staying informed about audit trends and implementing robust compliance strategies, home health and hospice providers can navigate the complex regulatory landscape more effectively and focus on what matters most – delivering high-quality care to patients in need.
Introduction
In the ever-evolving landscape of home health and hospice care, staying compliant and avoiding claim denials is crucial for providers. Recent audit trends reveal persistent challenges in documentation, face-to-face encounters, and medical necessity justification. This comprehensive guide explores these trends and offers strategies for providers to enhance their compliance and documentation practices.
Home Health Audit Trends
Recent data from Centers for Medicare & Medicaid Services (CMS) contractors reveals several key areas where home health providers face claim denials:
1. Medical Necessity for Skilled Nursing Services
Surprisingly, the top reason for denials is related to the medical necessity of skilled nursing services. This shift indicates that auditors are increasingly scrutinizing the actual content of clinical documentation rather than just technical requirements.
2. Face-to-Face Documentation Issues
Despite being in place for over a decade, face-to-face documentation remains a significant challenge. Providers often struggle with: - Missing or incomplete documentation - Untimely encounters - Lack of clear connection between the encounter and the reason for home health services
3. Plan of Care and Certification Problems
Issues with initial certifications, including missing, incomplete, or invalid documentation, continue to be a major cause of denials.
4. Therapy Services Documentation
Even with the removal of therapy thresholds in the Patient-Driven Groupings Model (PDGM), auditors still focus on the medical necessity and complexity of therapy services.
5. Timely Submission of Medical Records
A significant number of denials occur simply because providers fail to submit medical records within the required 45-day timeframe.
Hospice Audit Trends
Hospice providers face their own set of challenges in avoiding claim denials:
1. Terminal Prognosis Documentation
The top reason for hospice denials is insufficient documentation supporting a terminal prognosis of six months or less. This highlights the need for comprehensive, ongoing documentation of the patient's condition and trajectory.
2. Election Statement Issues
Technical problems with hospice election statements, including missing elements or incorrect dates, account for a large portion of denials.
3. Face-to-Face Encounter Requirements
Similar to home health, hospice providers struggle with meeting face-to-face encounter requirements.
4. Timely Submission of Medical Records
As with home health, failure to submit records in a timely manner is a significant issue for hospice providers.
Strategies for Improving Compliance and Reducing Denials
To address these audit trends and minimize the risk of claim denials, providers should focus on the following areas:
1. Enhance Documentation Practices
- Train staff to provide detailed, patient-specific documentation that clearly demonstrates medical necessity - Implement regular internal audits to identify and address documentation gaps - Utilize technology solutions to streamline and improve documentation processes
2. Strengthen Face-to-Face Encounter Processes
- Develop clear protocols for obtaining and documenting face-to-face encounters - Educate referring physicians on the importance of thorough documentation - Implement a system to track and follow up on missing or incomplete face-to-face documentation
3. Improve Physician Collaboration
- Establish strong relationships with referring physicians and educate them on documentation requirements - Develop a process for gentle but persistent follow-up to obtain necessary signatures and documentation - Consider using technology solutions to facilitate easier communication and document exchange with physicians
4. Implement Robust ADR Response Processes
- Create a clear workflow for handling Additional Documentation Requests (ADRs) - Designate specific staff members responsible for managing ADR responses - Set up a system to track deadlines and ensure timely submission of requested documentation
5. Leverage Technology for Compliance
Providers should consider implementing advanced technology solutions, such as RapidClaims, to enhance their coding and documentation processes. RapidClaims' AI-powered coding solution can help: - Streamline the coding process, reducing the risk of errors and omissions - Ensure higher accuracy in translating clinical documentation into precise medical codes - Improve team efficiency by automating routine tasks - Enhance compliance with the latest coding standards - Optimize revenue cycle management by reducing coding-related denials
Conclusion
As audit trends in home health and hospice continue to evolve, providers must stay vigilant and proactive in their compliance efforts. By focusing on comprehensive documentation, improving physician collaboration, and leveraging technology solutions like RapidClaims, providers can significantly reduce their risk of claim denials and ensure they receive appropriate reimbursement for the vital services they provide. Remember, compliance is an ongoing process that requires continuous attention and improvement. By staying informed about audit trends and implementing robust compliance strategies, home health and hospice providers can navigate the complex regulatory landscape more effectively and focus on what matters most – delivering high-quality care to patients in need.
Rejones Patta
Rejones Patta is a knowledgeable medical coder with 4 years of experience in E/M Outpatient and ED Facility coding, committed to accurate charge capture, compliance adherence, and improved reimbursement efficiency at RapidClaims.
Latest Post
Top Products
%201.png)